Conditions

Protection matters
In Conditions
Bookmark
Record learning outcomes
Incidence rates of skin cancer continue to rise, particularly among young people. But what’s behind this increase and how can customers protect their skin?Â

Skin cancer is one of the most common types of cancers in the world, with more than 100,000 new cases being reported each year in the UK alone. “Skin cancer is becoming more common because we have more sun exposure, more access to travel abroad and more leisure time,†says Dr Catherine Harwood, consultant dermatologist at Barts Health NHS Trust and spokesperson for the British Association of Dermatologists. Better diagnosis, higher levels of awareness and spending more time in sunnier climes are all contributory factors to the rise in incidence, but what’s the actual cause of the disease?
The main cause of all types of skin cancer is over-exposure to UV light – either naturally from the sun or artificially from sunbeds and sunlamps. Sunlight is the primary culprit and is made up of three types of UV – A, B and C. UVC is filtered out by the Earth’s atmosphere, so doesn’t affect us, but with prolonged or continued exposure, UVA and UVB can damage the skin. “In general, UVA stands for ‘age’ and UVB for ‘burn’,†says Aine McCarthy, science information officer at Cancer Research UK.
However, we can’t differentiate between the two. UVA consists of longer wavelengths and makes up around 95 per cent of the sun’s rays. While UVB causes the majority of skin damage, both UVA and UVB rays suppress the skin’s ability to repair itself once the damage has been done.
“UV exposure causes a level of immunosuppression in all individuals because it inhibits the immune cells from responding to DNA damage,†says Dr Harwood. When skin burns, blood vessels dilate and chemicals that lead to inflammation are released. “Our skin has evolved over time to adapt to the UV that constantly surrounds us,†explains Dr Harwood.
“Peeling occurs because of cell death as a way of the body rejecting cells that are damaged beyond repair. However, if damaged DNA remains in cells and divides, it can cause cancer.†Anyone can develop skin cancer, but it becomes more common with age.
Other risk factors include having:
- A personal or family history of the condition
- Pale skin that burns easily
- Fair eyes or hair
- A large number of moles or freckles
- A pre-existing condition that suppresses the immune system (e.g. AIDS)
- Taking immune-suppressing medication (e.g. chemotherapy)
- Prior exposure to certain chemicals (e.g. creosote and arsenic).
Skin should be checked regularly to monitor for changes because early diagnosis of skin cancer can help to ensure successful treatment and prevent the cancer from becoming advanced or spreading to other parts of the body.
What is skin cancer?
Non-melanoma
“Non-melanoma skin cancer (NMSC) is the most common form of cancer in the UK and the most common form of cancer globally among Caucasian populations,†says Dr Harwood. Around 102,000 cases of NMSC are diagnosed each year in the UK, making it the most common type of cancer by far. However, many cases go unrecorded or are only noted the first time they occur in recurring cases.
“It’s probably around two to three times more common than is recorded,†says Dr Harwood. NMSC refers to a group of cancers that develop slowly in the upper layers of the skin. The first sign is usually the appearance of a lump or patch that doesn’t heal after several weeks.
These normally develop on commonly exposed areas of skin, such as the face, hands, ears and shoulders. NMSC is defined depending on the skin cell the cancer originates in. “Skin is made up of the upper layer, which is the epidermis and the lower layer, which is the dermis,†explains Aine.
“The upper layer consists of a mixture of basal cells, melanocytes and keratinocytes. Genetic faults or mistakes that occur in the basal cells lead to the development of basal cell carcinoma (BCC) and faults in the keratinocytes cause squamous cell carcinoma (SCC).†BCC accounts for around 75 per cent of skin cancer cases, while SCC makes up around 20 per cent.
BCC usually appears as a small red lump that may be pearly or ‘waxy’. However, they can also be red, scaly patches. These develop slowly and may bleed, crust or develop into painless ulcers.
“There’s a lot of diagnostic confusion,†says Dr Harwood. “BCC often gets mistaken for ringworm, a patch of eczema or scarring.†In contrast, SCC develops more quickly and appears as firm, pink lumps that may have a flat, scaly or crusted surface.
These often bleed easily, are tender to touch and may ulcerate. “In very general terms, high intensity episodes of sun exposure are associated with BCC, while SCC is more associated with chronic exposure, for instance if you work outdoors or have an outdoor hobby,†explains Dr Harwood. Although BCC is easy to treat, it can cause a huge amount of morbidity.
“BCC tends to develop on cosmetically exposed sights so is often very visual, with surgery leading to scarring and skin grafts,†explains Dr Harwood. “However, most deaths are from SCC, which kills around 500 to 600 people every year in the UK.†Surgery is the main treatment option and is successful in more than 90 per cent of cases due to the low risk of NMSC spreading to other parts of the body (known as metastasized).
For instance, SCC spreads in two to five per cent of cases, while BCC is lower still, spreading in just 0.5 per cent of cases. However, NMSC can return, particularly if it was widespread or severe, so regular check-ups are important.
Melanoma
“Melanoma is a more aggressive form of skin cancer and causes around 75 per cent of skin cancer deaths,†says Dr Harwood. “If caught early enough, it can be treated effectively. However, it’s very hard to treat once it becomes metastatic or advanced.â€
Melanoma most commonly develops on the back, legs, arms and face. The most common sign is the emergence of a new mole or a change to an existing mole. Normal moles are usually round or oval with smooth edges and measure no more than 6mm in diameter.
Although melanoma is a relatively rare form of skin cancer, it is becoming increasingly common, with around 13,300 new cases diagnosed each year in the UK. It is one of the most common types of cancer in people aged 14 to 34, with more than a third of cases occurring in people younger than 55. What’s more, it claims more than 2,000 lives each year in the UK.
“Treatments are advancing, but they extend life rather than curing the disease,†explains Dr Harwood. “Melanoma kills a disproportionate number of young people (under 45 years old) and causes a disproportionate number of life years lost.†The reasons why melanoma or NMSC develop are complex.
“It’s largely due to genetic programming – what may be an inadequate length of UV exposure for one, may not be a problem for another,†explains Dr Harwood. “There’s also an element of bad luck – it often depends on what sun ray falls on what skin cell.â€
According to Aine, nonhereditary mutations in the BRAF gene are responsible for around 50 per cent of melanoma cases, while having lots of moles (more than 50) and at least one family member with melanoma (known as familial atypical multiple mole melanoma syndrome (FAMMM)) accounts for around 10 per cent.“This means an individual has lots and lots of moles, which makes them more susceptible,†explains Aine.
 It is particularly important to protect babies and young children from the sun
It is particularly important to protect babies and young children from the sun
Â
Â
Protect to prevent
Pass on the following advice to help keep customers sun safe this summer:
- Wear a broad-spectrum sunscreen of at least SPF30 – waterproof if necessary
- Apply sunscreen approximately 15 minutes before sun exposure
- Reapply sunscreen every two hours – more if swimming or towel drying
- Avoid the sun between 11am and 3pm
- Cover up exposed areas of the skin with clothing
- Wear a hat that protects the face and scalp
- Wear CE or British Standard marked sunglasses. Ensure they have a UV 400 label and offer 100 per cent UV protection
- Take extra care with babies and young children, and encourage them to play out of the direct sunlight.
Â
The safe side of sun
An area of ongoing research that has recently received much media coverage is the importance of an adequate and regular supply of vitamin D, which is primarily obtained via UV exposure and is difficult to achieve through diet alone. “It’s not clear how much sun exposure we need [to supply us with sufficient vitamin D] and it certainly varies according to skin type, time of year and latitude,†says Dr Harwood. “But people really don’t need to burn – it’s easy to take a supplement.â€
Dr Harwood also advises people to be wary when getting 10 to 15 minutes of unprotected sun exposure a day, as has been previously recommended by a number of organisations. “The guidelines may be up to 15 minutes a day, but 15 minutes for a fair-skinned person in Brisbane is different from an Indian person in Stockholm,†she says. “Don’t give out blanket advice.†When it comes to tanning, experts agree that there is no truly safe way, but that doesn’t mean people can’t enjoy the summer months.
“You shouldn’t stop going to the beach or swimming in the sea, but don’t lie in the sun specifically to get a tan,†says Dr Harwood. “A tan is a sign that the skin is trying to repair itself by making its own ‘sunscreen’. Pigment cells produce melanin, which gets shunted into cells to protect the cell nucleus.â€
 Melanin is produced by skin cells called melanocytes and offers some protection by absorbing UV radiation, which makes the skin turn darker. However, its protective capabilities are limited. “Skin cancer does occur in olive and dark skin tones, so it’s vital to protect yourself,†says Aine.
“No one should lie in the sun for eight hours.†As for the belief held by some that sunbeds offer a certain degree of protection, Dr Harwood insists that any benefit is negligible. “At an absolute maximum, it’s the equivalent of SPF6 and we would never advise anybody to use an SPF6 sunscreen,†she says.
Despite the many known dangers of UV exposure, Dr Harwood admits that delivering the ‘safe sun’ message to younger generations is particularly challenging. “Younger age groups think they’re going to live for forever and they’re never going to get cancer, so any health campaigns just bounce right off them,†she says. Instead Dr Harwood recommends that pharmacy teams advise people on protecting themselves from the sun’s ageing effects, which in turn will help to prevent skin damage.
“The message about skin cancer doesn’t sink in like the message about ageing,†she believes. “I see nothing wrong with advising people on how to reduce their risk of ageing, which at the same time will reduce their risk of skin cancer.â€
Â
Keep an eye out
“Moles don’t have a particular cancer potential, but they can ‘turn on’ and increase the risk of melanoma,†says Dr Catherine Harwood, consultant dermatologist at Barts Health NHS Trust and spokesperson for the British Association of Dermatologists. Advise customers to follow Cancer Research UK’s ABCD guideline to detect potentially troublesome moles (see images below) and refer to the pharmacist anyone with a lump, lesion or skin discolouration that hasn’t healed after four weeks.
Asymmetry
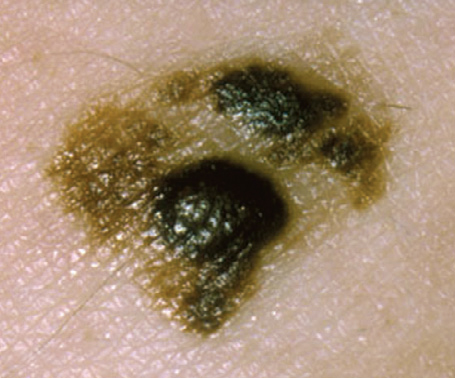
The two halves of the mole not looking the same.
Â
BorderÂ
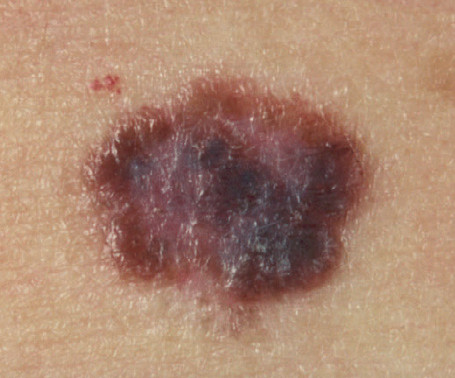
Irregular, blurred or jagged edges
Â
Colour
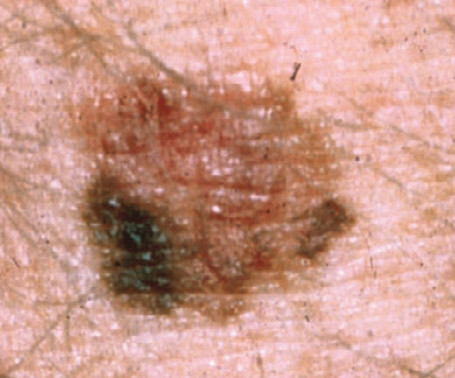
Uneven colouration with one or more shade.
Â
Diameter

Wider than 6mm in diameter.
A tan is a sign that the skin is trying to repair itself by making its own ‘sunscreen’
