Conditions

Gains without shame
In Conditions
Bookmark
Record learning outcomes
 Community pharmacy has tended to shy away from HIV patients, but with well over 100,000 people in the UK now living with the condition, it is time to step up.Â
Community pharmacy has tended to shy away from HIV patients, but with well over 100,000 people in the UK now living with the condition, it is time to step up.Â
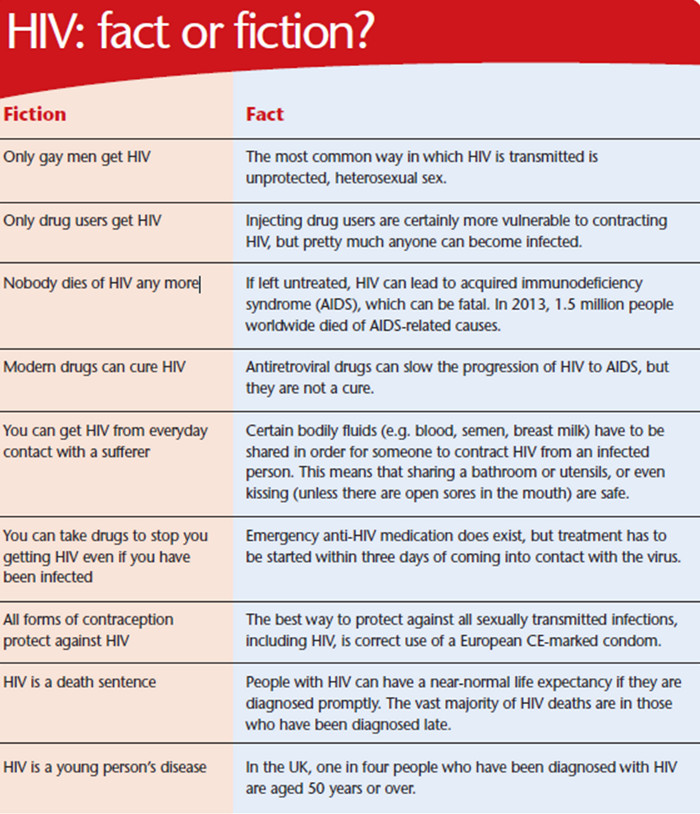
The human immunodeficiency virus – more commonly known as HIV – might seem irrelevant to most people, but a report published recently by Public Health England stated that almost 111,000 people in the UK were living with the condition in 2013. This means that just under two in every thousand women and just under four in every thousand men have HIV, and a quarter of these – that’s more than 25,000 people – are thought to be unaware of this fact. Perhaps HIV is a little closer to home than most like to think.
Traditionally, HIV testing and treatment have been the realm of hospital clinics, but as the condition is starting to become better understood, certain aspects are starting to filter into primary care. An important step in this direction took place last April when it became legal to sell HIV home testing kits in the UK. Heather Leake Date, consultant pharmacist for HIV and sexual health at Brighton and Sussex University Hospitals NHS Trust, explains: “Prior to this, people could do a home test where they sent a sample to a lab and received the result by phone or email, etc, whereas the new home HIV kits are like pregnancy tests in that someone can buy one to do at home and get the results there and then.â€
The differences in these test types means pharmacy staff need to be aware which they are selling so they know when to provide information, says Heather, who is a member of the HIV Pharmacy Association’s (HIVPA) expert panel: “Someone who uses a home HIV test might only see a health professional at the time they buy it, so it is important they are provided with information on local sexual health services so they can follow up their result.â€
This might only seem relevant if the individual gets a positive result, but Heather warns against making this assumption: “Someone who gets a negative result could think they don’t need to do anything else, but it might be a good idea for them to be tested for other sexually transmitted infections or maybe have a full sexual health screen.â€
There may be some people who think that pharmacy isn’t the right place for HIV testing to take place, but Heather is firm in her belief that it is. “We really need to offer HIV testing in as many different places and ways as possible in order to reduce the pool of undiagnosed patients, and pharmacy is the perfect place for people who might feel uncomfortable going elsewhere,†she says. “The main thing is that staff have to be fully trained and supported so they know how to make the best of any opportunities that arise.â€
Moving on from testing
Once someone is diagnosed as HIV positive, they are referred for specialist care and may be put on to medication to try and delay or stop the virus attacking their immune system. For many years, provision of these drugs has generally been done through homecare companies, but Superdrug’s Newport branch is bucking the trend.
Pharmacy manager Tim Morgan explains: “Since late 2011, we have been dispensing HIV drugs for patients who attend the clinic at the nearby Royal Gwent Hospital.†The pharmacy now has close to 200 patients on its books, all of whom can benefit from the other services on offer, including a medicines use review (MUR) tailored to their specific needs.
It isn’t just pharmacists who are involved in all of this, says Tim, who is also a service development manager for Superdrug: “Staff are an essential part of the ordering and dispensing side of things, which leaves me and second pharmacist Claire Taylor clear to deal with the more clinical aspects.†Stock management is far from straightforward, Tim adds, because many of the drugs have to be ordered directly from the manufacturers, all of whom have their own way of doing things. “It is the most time consuming and stressful part of the service,†admits Tim, who is hoping he will be able to provide an extra level of support to patients once he has completed his independent prescribing course.
The two pharmacists and accuracy checking technician Keri Jones-McDonald have taken things a step further by becoming members of the HIVPA, and Keri is in charge of the scheme when locums are working to ensure continuity for patients. Tim says her skills and knowledge are second to none: “Keri has made some really impressive interventions, such as spotting drug interactions and incorrect doses.†The service itself has also not gone unnoticed, winning an innovation award at the 2014 Clinical Pharmacy Congress. Such a comprehensive service is probably outside the scope of many pharmacies, but with so many patients on HIV medication, everyone working in the sector needs to be aware that these drugs have the potential to interact with many other medicines.
Heather says: “Some of the most common are antacids, statins, supplements, fluticasone nasal spray and other inhaled steroids.†While it is part of the standard sales protocol to ask someone buying an OTC product if they take any other medication, Heather says that for HIV patients, the way in which they are asked can really matter: “If they are in the middle of a crowd of people at the counter, they might not want to say what they are on, whereas having a poster up or maybe a laminated sheet on the counter – maybe one that says “Ask to speak to the pharmacist if you are on any of these medicines†and lists the antiretroviral drugs – might make it easier for people to communicate the information.â€
A sensitive issue
HIV is, of course, a good fit with other sexual health services provided by pharmacies, which, in turn, can complement each other. Bowness Pharmacy in Middleton, for example, mentions its chlamydia and gonorrhoea screening service to anyone who enquires about its emergency hormonal contraception (EHC)scheme. Pharmacist and owner Prak Jha says: “We tell people that they need to pee in a pot, which we label and send off to a lab, and just talk about it as just another bacterial infection rather than some horrible sexual disease.
This means we don’t get their backs up and they are much more likely to get tested.†Prak adds: “It’s all about mindset and approach. The counter staff are sensitive to the fact that people might be embarrassed, so get them into the consultation room where they can talk more freely.†The staff at the Numarkmember pharmacy have benefited hugely from training provided by RUClear?, an NHS-run organisation that offers gonorrhoea and chlamydia testing to young people in several parts of the UK, including the Greater Manchester area, says Prak.
Paul Casey, training manager at the sexual health charity FPA, agrees that EHC requests can be an effective opening for other sexual health topics. “It is best to keep it general, so ‘Was there anything else about your sexual health you wanted to talk about?’ can be a good way to encourage someone to open up and have a wider conversation.†He adds: “Some people worry about straying outside their area of competence, but in reality what they usually end up doing – and pharmacy is excellent at this – is signposting to services and information, and letting people know what is available locally.â€
Paul says it is worth giving a little thought to practical issues: “Putting up a poster that says ‘Want to talk to someone about your sexual health? We have a private room’ is a good way of letting people know that the pharmacy is a place where such conversations can be held.†But he warns against making assumptions about people’s lifestyles: “Not everyone in need of sexual health advice is young, straight or married. Make sure you, and any materials you use, are inclusive in terms of who is having sex with whom.â€

Pharmacy has come a long way since selling condoms was the only sexual health service it provided
The future
Pharmacy’s offering in the sexual health arena is only set to grow. Over at Superdrug, plans are afoot to try and integrate the company’s online doctor service, which – unsurprisingly – deals with a large number of prescriptions for erectile dysfunction, chlamydia and unprotected sexual intercourse – with the skills of its pharmacists and the growing number of instore, nurse-led clinics. Tim says: “We are always looking to make services more accessible and offer more advice.†At Bowness Pharmacy, staff aren’t waiting for people to come to them, but instead are going out and about to spread awareness of sexual health issues.
Prak says: “Every eight weeks or so, three members of staff and I run a stall at a health fair run by our local community centre. We are there all day doing free health checks, which include sexual health, and can signpost people to the pharmacy if they need something more. The health fairs take place in a wide range of locations, from supermarkets to Sure Start centres, and are really well publicised so we can see 120 people in one day!†As for HIV, it has come a long way since the 1980s when it was pretty much viewed as a death sentence.
HIVPA’s Heather comments: “It is now considered a long-term condition, with people expected to live a fairly normal lifespan, and there is also an ageing population so we are seeing people with HIV and other conditions such as high blood pressure and diabetes. This means that the chances of them being on other medicines is very high, and so we need to improve the two-way communication between hospitals and clinics, where HIV is managed, and primary care – which includes GPs and pharmacies – where much of the care of these other conditions takes place.â€
Pharmacy has certainly come a long way in the last couple of decades. While condoms used to be kept on or even behind the counter and customers asked for them in hushed tones, now staff are confident in offering advice and clinical services to patients who are comfortable asking for information and accessing what is on offer. HIV is maybe the final frontier of sexual health, but it’s one that pharmacy is well equipped to take on.
Â
Common STIs
Sexually transmitted infections (STIs) are passed from one person to another through unprotected sex or genital contact.
Chlamydia
Chlamydia is one of the most common STIs in the UK, but most people will not experience any symptoms so are unaware they are infected. In women, the infection can cause pain or a burning sensation when urinating; vaginal discharge, and pain in the lower abdomen during or after sex, or between periods. It may also cause heavy periods. In men, it can cause pain or a burning sensation when urinating; a white, cloudy or watery discharge from the tip of the penis, and pain or tenderness in the testicles. The infection can be diagnosed via a urine test or a swab of the infected area and it can be easily treated with antibiotics. If left untreated, however, it can lead to serious long-term health problems, including infertility.
Genital warts
Caused by the human papilloma virus (HPV), genital warts are small, fleshy growths, bumps or skin changes on or around the genital and/or anal area. Although usually painless, they can cause itching, redness and occasionally bleeding. Spread by skin-to-skin contact alone, the infection can be treated using creams and cryotherapy (freezing the warts).
Genital herpes
Genital herpes is caused by the herpes simplex virus (HSV), which is the same virus that causes cold sores. Symptoms usually include small, painful blisters or sores, which may itch, tingle or make urinating painful. Just like cold sores, once someone has been infected, the virus remains dormant until reactivated by a trigger that causes the blisters to develop again (although they’re usually smaller and less painful). There is no cure for genital herpes, but symptoms can usually be controlled using antiviral medicines.
Gonorrhoea
About 50 per cent of women and 10 per cent of men don’t experience any symptoms with gonorrhoea, a bacterial STI that’s easily passed on during sex. If symptoms do occur, in women they can include pain or a burning sensation when urinating; vaginal discharge (often watery, yellow or green); pain in the lower abdomen during or after sex; bleeding during or after sex or between periods, and sometimes heavy periods. In men, the infection can cause pain or a burning sensation when urinating; a white, yellow or green discharge from the tip of the penis, and pain or tenderness in the testicles. Diagnosed using a urine test or a swab of the area, the infection can be easily treated with antibiotics. Again though, if left untreated, it can lead to more serious, long-term problems, including infertility.
