Conditions

Ahead of the game
In Conditions
Bookmark
Record learning outcomes
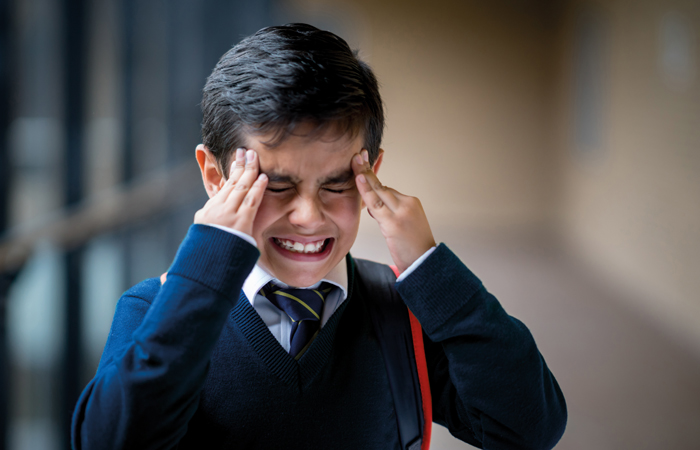
Headaches and migraine are often regarded as adult-only problems, but most children experience these ailments at least once a year, and many suffer regularly
Look at the shelves of any pharmacy and pain relief products feature prominently. Often packaged in red cartons to maximise their presence while simultaneously sending a subliminal message that these products mean business, the analgesic category isn’t shy in asserting its dominance.
And dominant it is. According to the Proprietary Association of Great Britain (PAGB) – the trade association that represents manufacturers of OTC products, devices and food supplements – pain relief is the biggest OTC category, with value sales of £576.9 million in the year ending 23 April 2016. To put this into perspective, the next biggest category is cough, cold and sore throat, which had value sales of £415.1 million. This means that the British public spends £150 million more on pain relief than they do on coughs and colds every year. And this spending is increasing – sales of OTC analgesics were up 1.85 per cent during 2015-16.
When you look at where the growth is coming from, it’s interesting to note that it’s not from pills taken by adults – sales of adult oral pain relievers actually declined by 0.5 per cent during the year. Instead, the growth is coming from topical and paediatric analgesics. When it comes to headache in children, research from Nurofen for Children manufacturer RB shows that 71 per cent of parents turn to pharmacies for advice, yet there is a lack of confidence when it comes to managing the condition and knowing when to refer a child for medical advice.
How common is headache in children?
Headaches are often considered a problem that only affects adults, but Susan Haydon, who runs The Migraine Trust’s Information and Enquiry Service, says: “Around 70 per cent of schoolchildren have a headache at least once a year. One in four of these children suffer from recurrent headaches.”
Dr Andrew Dowson, director of headache services at King’s College London, adds: “The type of headaches experienced by children is different to adults – they tend to be lower grade and less frequent.”
Children are masters at deteriorating at an alarming rate and then quickly bouncing back, which makes it tricky for pharmacists and team members to know when to advocate a ‘wait and see’ approach and when to refer them for medical attention. Dr Dowson instructs: “If the headache is their first or worst, refer them to their GP or one of the NHS helplines. If there are specific symptoms that ring alarm bells – a stiff neck and an aversion to lights that suggest meningitis, for example – send them to accident and emergency. Always bear in mind the principle ‘first do no harm’ – it is safer to refer if you are unsure.”
In terms of distinguishing what type of headache the child is suffering from, Dr Dowson advises considering the impact it is having. “If it is not disrupting the child’s activities and there aren’t any other issues – for example, nausea or dizziness – it is probably a tension-type headache. Lifestyle factors are likely to be at play, such as dehydration, missing meals or stress, and it will usually pass quite quickly. If the headache is causing disruption, it tends to be a migraine, although a diagnosis is unlikely to be made before the child has had five attacks. An exception is made if aura is experienced – i.e. disturbances to eyesight or speech, or other neurological symptoms such as tingling, dizziness, numbness or weakness. If that is the case, it is always regarded as migraine.”
Susan expands: “Migraine affects children slightly differently to adults, in that the pain often affects the whole head rather than just one side. Attacks are usually shorter, and sickness, vomiting or abdominal pain may be the dominant symptom rather than headache.”
Other headache types, such as cluster headaches – characterised by sudden and severe pain on one side of the head, often around the eye – are rare in children, so any suspected cases always warrant referral to a GP. Medication overuse headache, however, is a different matter, explains Dr Dowson: “It stems from analgesic dependence, which in adults is more common with codeine or caffeine, but in children is more likely to be from paracetamol or ibuprofen.”

Aura and red flag symptoms
Migraine with aura can have non-headache symptoms, including:
- Visual disturbances such as flickering lights, spots or lines, and partial loss of vision
- Sensory changes such as pins and needles, or numbness
- Speech disturbances.
The patient (or parent or carer) is usually the best person to determine if what they are experiencing is normal for them, but anything that persists for longer than expected and certainly for more than an hour should be referred for medical advice.
The following are not usually aura symptoms, so also need referring: muscle weakness; double vision; visual symptoms affecting only one eye; poor balance; decreased consciousness, difficulty waking or seizures; abnormal head position; recurring headache, particularly on waking and with nausea or fever; headache that gets worse over several weeks; rash, and stiff neck.
Using supplements to prevent migraines
Dr Andrew Dowson, director of headache services at King’s College London, says that certain supplements and aspirin can help some people suffer from fewer migraines. “Vitamin B2 at a dose of 400mcg a day, magnesium 400mg, co-enzyme Q10 100-300mg and aspirin 75mg have all been shown to affect serotonin levels in the brain, so can make a difference,” he says. “The aim is to reduce the number of affected days by 50 per cent. For most of these supplements, if they are going to have this effect, it should happen within a month or so. The only exception is vitamin B2, which should be tried for three to four months before deciding whether it is having any benefit.”
What to do
Management of tension-type headaches is straightforward. Any triggers that are likely to be causing the problem should be resolved if at all possible. This may mean making sure that the child sips regularly from a water bottle while they are at school so they don’t become dehydrated, or making sure they have breakfast to prevent hunger if there is a danger they may skip lunch. Suitable simple analgesics may be given if needed.
It is of course advisable to avoid triggers for migraine too, although Susan cautions that migraine can be an unpredictable condition. “Parents and children learn from experience that certain things can trigger an attack, but the influence of these triggers is complicated,” she says. “On one occasion, a known trigger will appear to bring on a migraine, yet on another it has no such effect. This suggests that a certain combination of factors together may be necessary to trigger an attack.”
Common triggers include sleep (too much as well as too little); not drinking enough; lack of food or eating sugary snacks instead of balanced meals; sudden exercise, and computer screen glare and flicker. Susan recommends establishing a regular routine for children as this can lead to less frequent migraine attacks. Factors such as environmental issues (e.g. bright lights) and food triggers can be difficult to manage, but keeping a diary can help to identify them. It is also useful to make a note of warning signs that a child is about to succumb to a migraine. Such signs could include tiredness and yawning, muscle pain, pale complexion, altered behaviour, confusion and food cravings.
When it comes to exercise, it’s all about finding a balance. Some people find that sudden exertion can bring on a migraine, which may make them opt for a sedentary lifestyle. But there is some research that suggests that moderate exercise can reduce the frequency and severity of migraine attacks in some people, so a better approach is to find an activity that the person enjoys and then gradually increase its duration and intensity. Warming up and cooling down are crucial in preventing muscle tension, which can trigger migraine and headache, as are eating sensibly to avoid blood sugar lows and staying well hydrated before, during and after exercise.
Dr Dowson says that taking medication to relieve symptoms is important in the management of migraine. “Non-steroidal anti-inflammatory drugs are better than paracetamol here, and need to be taken as early as possible in the headache phase,” he advises. “Medication that may be prescribed includes triptans and metoclopramide, although there are restrictions and warnings on using these drugs in children.”
Science, not fiction
Transcutaneous electrical stimulation of the supraorbital nerve for the treatment and prevention of migraine may sound like science fiction, but it is in fact something that was approved by the National Institute for Health and Care Excellence (NICE) in 2016. And there are no scalpels involved. The patient simply wears a headband device called Cefaly, which stimulates the nerves under the skin of the forehead, much like a transcutaneous electrical nerve stimulation (TENS) machine that could be worn for back pain. In its assessment, NICE said that it had received a lot of positive patient accounts about the device, and that it might be particularly useful for those who did not want to take medication or who could not tolerate it.
The device isn’t cheap, retailing at £249, but there is a 60-day cooling off period, so anyone who doesn’t get the benefi t that they are hoping for and returns the product according to the manufacturer’s terms and conditions receives a significant portion of their money back.
What about teenagers?
As if the teenage years aren’t angst-ridden enough, this time of life introduces a whole range of extra factors that can cause headaches – and migraine in particular.
Many of the triggers already mentioned may be heightened – a constant stream of deadlines for coursework as well as tests and exams are stressful for even the most chilled out individual. Similarly, eating habits can become erratic and drinking water falls down the list of priorities. Hormones can also have a significant impact, with 50 per cent of girls with migraine saying their attacks are linked to their menstrual cycle. Hormonal contraceptive methods can be problematic too. That isn’t to say that migraine sufferers can’t go on the contraceptive pill or similar, but it certainly needs to be taken into consideration when deciding on the best method of birth control. Alcohol, smoking and drugs can also increase vulnerability to an attack, particularly for people who are tired and dehydrated, Susan warns.
It’s really important to get a handle on migraine. Otherwise, the impact it can have on the sufferer’s life can be enormous. “As well as the physical pain and discomfort of an attack, some migraine symptoms can be quite frightening,” says Susan. “The child may become anxious about having a migraine and opt out of activities that they fear may bring on an attack, or miss school or other pursuits because of an episode. This not only means their education may suffer, but it can also leave them feeling frustrated and ‘different’. If their social life suffers, they may develop feelings of low self-esteem.”
Further information
- The Migraine Trust is a charity that has been championing migraine research and supporting those affected by the condition for over 50 years
- NHS Choices – children’s headaches
- The National Institute for Health and Care Excellence (NICE) has published guidance on the diagnosis and management of headaches in over 12s
- The National Migraine Centre differs slightly to many other medical charities as it provides a diagnosis and treatment service for migraine and headache sufferers.
71 per cent of parents turn to pharmacies for advice on childhood headaches
