In Conditions
Follow this topic
Bookmark
Record learning outcomes
The body’s largest and most sensory organ, the skin, plays an enormous role in one’s health – tasked with being the first line of defence against potential irritants, bacteria and injury. “The skin is crucial to our overall wellbeing; from keeping the body separate from the world outside to maintaining a vital part of our sense of ‘self’,” says consultant dermatologist and British Skin Foundation (BSF) spokesperson, Dr Anthony Bewley.
Layer up
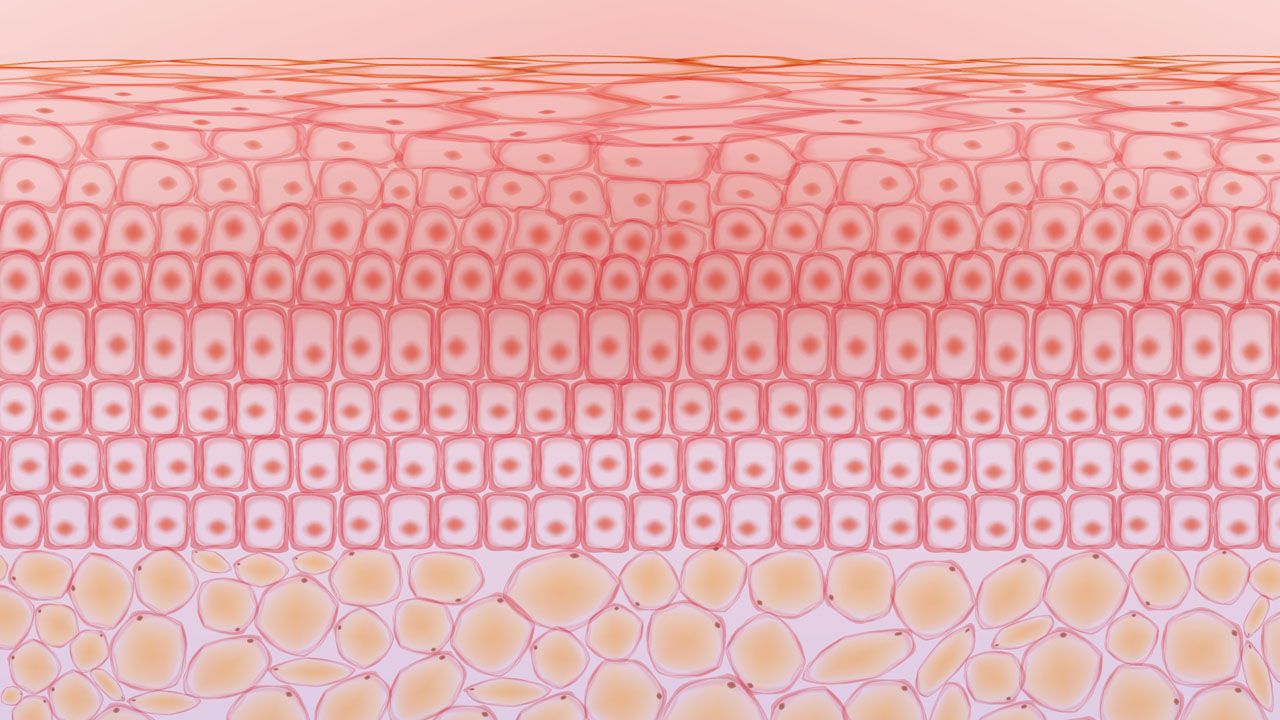
The skin is made up of three layers, the epidermis, the dermis and the sub-cutaneous layer or hypodermis. Characterised by elasticity, the epidermis, the outer layer of the skin, is constantly being regenerated and is home to pores which allow oil and water to escape. It is the only layer of skin which is visible to the eye.
The dermis, the inner layer, contains oil glands, hair follicles, connective tissues and lymph vessels. It is responsible for temperature regulation and producing sebum (an oil) which combines with sweat to keep dust and bacteria away from hairs.
Made up of connective tissue and fat, the sub-cutaneous layer or hypodermis lies under the dermis. It is the deepest layer of skin with the primary task of insulating the body and protecting the internal organs and muscles from external physical injury and/or temperature changes.
Between detecting touch and temperature, producing vitamin D and regenerating itself, the skin is constantly working – making it no surprise that from time to time, and for some people more often than not, the skin requires a bit of attention. As the most sensory organ reactive to changes in pressure, temperature, vibration, pain and pleasure, and as an ‘emotional’ organ that reacts to factors like stress or excitement, the skin is a fundamental aspect of good health.
There are a multitude of skin conditions people can develop, both acute and chronic, that pharmacy teams can provide advice and over-the-counter (OTC) options for.
Impacting impetigo
Impetigo is a bacterial infection of the skin causing sores and blisters to form on the skin’s surface. It is highly contagious, making early identification and treatment crucial. Children between the ages of two and five are most commonly affected, but anyone can get it. The infection usually begins in broken skin such as minor cuts, insect bites or rashes – which is why it is important to keep these ailments clean – although it can still develop in healthy skin. On white skin, it may appear as pink or red sores or patches, and on black or brown skin, it can appear as red, purple, brown or grey patches. When the blisters ooze or burst, they leave behind a yellowish crust and golden-brown patches. These sores or patches can be itchy as well as painful, but with treatment the condition betters after seven to 10 days.
Pharmacy teams can recommend various OTC solutions, such as a hydrogen peroxide or an antibiotic cream or ointment containing bacitracin, as well as self care advice to customers, such as:
- Staying at home
- Keeping sores/patches dry
- Washing all linen at a high temperature
- Wearing loose clothing
- Avoiding touching the sores to avoid scarring
- Washing hands frequently.

“Characterised by elasticity, the epidermis, the outer layer of the skin, is constantly being regenerated”
Looking after the lips
While many people take extra care to wrap up in winter or wear a hat in summer, they tend to forget about protecting their lips. As they tend to be more exposed to the elements than the rest of the body, lips can become dry and chapped. Dry air, wind, dehydration and sun damage are all reasons why this may happen. As lips have no oil glands, they cannot replenish moisture readily enough when they become dry. Customers should be advised to:
- Drink plenty of water
- Put on lip balm before going to sleep
- Avoid licking dry lips
- Use a lip balm with an SPF
- Avoid sharing lip products
- Avoid picking flaky lips
- Cover the mouth with a scarf or buff when outside in cold weather/extreme sunshine over a prolonged period.
Customers with hot, painful or swollen lips should be referred to the pharmacist as this may indicate an infection.
Taming flare ups
Eczema, also known as dermatitis, is a chronic, non-contagious condition affecting one in five children and one in 10 adults in the UK. The cause of eczema is not completely known, however, it tends to run in families and is common among those who also experience hayfever or asthma. Atopic eczema, the most common type, is caused by gaps in the skin cells that allow bacteria, irritants and allergens to penetrate the epidermis. These gaps also lead to increased water loss, meaning drier skin.
Atopic eczema tends to have ‘active’ and ‘inactive’ periods. Known as ‘flare-ups’ the active periods are acknowledged to be triggered by certain irritants. “Skin with eczema is more liable to become red and inflamed on contact with substances that are known to irritate or cause an allergic reaction,” explains the National Eczema Society. These differ for each person, but common triggers are fragranced detergents, perfumed soaps, stress, weather or certain materials.
On white skin, these affect the creases of body joints like the back of the knees or insides of elbows, while in darker skin tones, the front of the knees and outside of elbows are commonly affected. The skin becomes reddened on white skin or darker brown, purple or grey on brown skin and becomes itchy, scaly or cracked.
Emollients (moisturisers) are often the first thing recommended to treat flare-ups. Customers need to consistently use an emollient to help their dry skin. Topical steroids are also often recommended, as well as sedating antihistamines to help customers sleep at night, but long-term use of both of these medicines should be assessed by a GP. Pharmacy teams can suggest paste bandages or wet wraps to relieve itchiness and prevent scratching. Avoiding known triggers is one of the most effective ways of preventing flare-ups, and sometimes allergen tests can be recommended if a customer cannot pinpoint what is sparking their eczema.
A matter of the mind?
Chronic or visible skin conditions often coincide with mental health issues like stress or anxiety. Dermatologists and psychiatrists have recognised this link between skin and the mind as ‘psychodermatology’. Consultant dermatologist and British Skin Foundation (BSF) spokesperson, Dr Anthony Bewley, describes psychodermatology as: “Two sides of the same coin. It is either primary psychological or psychiatric disease which is skin focused (for example hair pulling disorders, skin picking disorders or body dysmorphic disorders), or it is skin disease which leads to psychological distress for example acne, eczema or vitiligo leading to changes in self-confidence, depression, anxiety or even suicidal thoughts.” There is still much to learn about this connection, but pharmacy teams can certainly implement a mindful and compassionate approach when dealing with people with skin conditions, bearing in mind the emotional and mental impact that can accompany their condition.
Scaled up
Psoriasis affects people with accelerated skin cell replacement, meaning they have an increased production of cells. “Usually, the skin replacement process takes 21-28 days, in people with psoriasis, this process is quickened and takes only a few days,” said a spokesperson from the Psoriasis Association. “While genetics and immune system issues are related, the precise role of genetics in psoriasis development is not fully understood.” This increased production of cells leads to patches of dry, scaly skin which appear in pink or red patches with white or silvery scales on white skin, and purple or dark brown patches with grey scales on brown or black skin.
Psoriasis can be treated with OTC products like topical creams and ointments, gels or shampoos, but depends completely on the severity of the psoriasis. Mild psoriasis benefits from applying emollients directly onto the skin to decrease water loss and cover the skin with a protective film, which also works to limit itching and scaling. Vitamin D analogue creams can be recommended for mild to moderate psoriasis. These creams are anti-inflammatory and decelerate the production of skin cells. Coal tar, another treatment option pharmacy team members can recommend, is one of the oldest remedies for psoriasis and relieves itchiness, scaling and inflammation. As it is a heavy, thick oil, customers should be warned that it can stain clothes and bedding.
If customers are not seeing improvements with these OTC treatments, they need to be referred to the pharmacist or GP.
Rock-a-bye baby
While some people develop skin conditions later on in life, some experience skin issues within their first few weeks. Seborrheic dermatitis, commonly known as cradle cap, is a common, non-contagious skin condition that affects infants usually between three weeks to 12 months. The condition forms over a baby’s scalp or forehead in yellowish, greasy scales and is caused by the overproduction of oil. This is thought to be due to the hormonal changes that occur during pregnancy which stimulate the infant’s oil glands, leading to overproduction.
Thankfully, it is a painless condition that disappears on its own after about six months. It doesn’t require treatment, but parents/caregivers can lightly massage an emollient onto the baby’s scalp to help loosen the scales, or gently brush the scalp with a soft brush before washing with baby shampoo to reduce the scales. It is important that shampoo is rinsed out thoroughly and no adult shampoo or oils are used. Pharmacy teams should also advise parents or caregivers not to pick the crusts as this can lead to infection. Unperfumed baby shampoos and gentle emollients should be recommended so as not to irritate the condition. If the condition spreads to other parts of the body or the scales look swollen, bleed or leak fluid, refer to the pharmacist.

Dig into dandruff
Another scalp condition is dandruff, which similarly to cradle cap, is not contagious and poses no real health threat apart from being uncomfortable and unpleasant. A common misconception is that dandruff is caused by poor hygiene, but it is in fact another impact of oil production on the scalp. Dandruff sufferers have a combination of a sensitive scalp, natural oils (sebum) and a scalp specific yeast-like fungus called Malassezia globosa which produces oleic acid. People with a sensitive scalp will react to this acid. During puberty, hormone changes increase oil produced by the scalp, making this a common period for people to develop dandruff symptoms for the first time. It can also be brought on by stress, old age (hormone changes) and weather conditions. Dandruff is characterised by white or grey flakes on the head or shoulders, but itching, redness and a dry scalp are also indicative of the condition.
Luckily, dandruff can be treated in the pharmacy and many shampoos have been designed to target it. Shampoos with any one of the following ingredients will help alleviate dandruff:
- Zinc pyrithione, which has antifungal properties
- Salicyclic acid, as it removes build-up
- Selenium sulphide, for severe cases, which contains an antifungal agent and should be rinsed out thoroughly to avoid discolouring the hair and scalp
- Ketoconazole, which kills dandruff-causing fungi
- Coal tar, or tar-based shampoos, as they slow down the rate at which skin cells die and flake off. These shampoos can make the scalp sensitive to sunlight
- Fluocinolone shampoos, known to reduce swelling, itching and flaking in severe cases.
Customers may need to alternate between medicated shampoos to maintain effectiveness. If symptoms are not improving or the scalp is red, swollen or symptoms have spread to the face or other body parts, refer the customer to the pharmacist.
“The cause of eczema is not completely known, however, it tends to run in families”
On the topic of treatment
Many skin condition treatments contain topical steroids. While highly effective as treatments, the skin can become dependent. Topical Steroid Withdrawal (TSW) occurs when moderate or high-potency topical steroids that have been used for a prolonged period come to an end. A higher potency steroid is sometimes required to alleviate these symptoms, which are often more severe than the symptoms initially experienced, and a dependency cycle is created. Many people experience red, dark, burning and itchy skin.
Pharmacy teams can advise customers to apply ice or a cool compress to the skin, recommend an antihistamine to relieve the redness and itch, pain relivers or non-fragranced emollients to soothe the skin. Furthermore, if customers come in to collect a prescription for a topical steroid cream, the pharmacy team can discuss the potential risks of TSW and ensure they have consulted all options. It is possible for people to see results on the smallest possible dose, or to alternate between nonsteroid and steroid medicine to avoid TSW in the long-term.