In Conditions
Follow this topic
Bookmark
Record learning outcomes
Many people take their eyes for granted – until something doesn’t seem right. Eye problems can cause a range of troublesome symptoms such as pain, headaches, itching or irritation and sight problems, having a significant impact on people’s daily lives.
In October 2019, a study conducted at City University London revealed that the public strongly valued their sight over their other senses. Yet research published in September 2024 for National Eye Health Week revealed that 19 million British people don’t have regular eye tests.
Dr Paramdeep Bilkhu, clinical adviser at The College of Optometrists, says that collaboration between optometrists and pharmacies is vital to improve people’s eye health. “Optometrists diagnose and manage a wide range of eye conditions and often direct patients to pharmacies for appropriate over-the-counter treatments, especially for dry eye, allergic conjunctivitis and bacterial conjunctivitis,” he says. “Pharmacies support patients in managing these conditions through expert advice, product selection and promoting safe self care.”
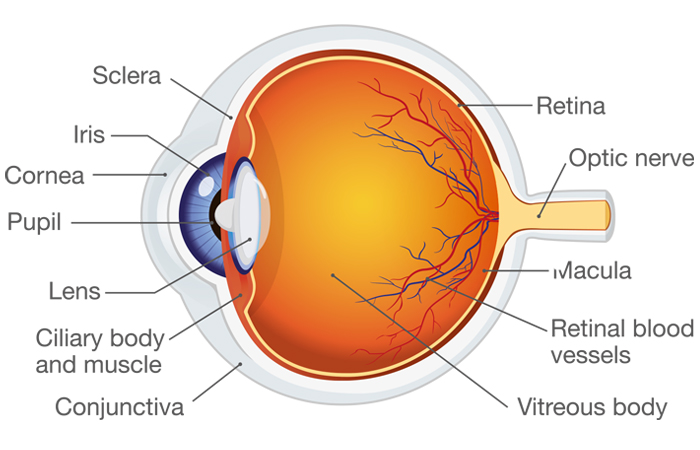
How the eye works
The human eye works in a similar way to a camera, turning light rays into images. This highly complex organ is made up of several different parts.
- Eyelids: These protect the front of the eyes and spread tear film
- Conjunctiva (thin membrane): This lines the inside of the eyelids to protect the eye and keep it moist
- Pupil (black circular hole): The pupil gets smaller in bright conditions and bigger in dark conditions, letting in different amounts of light. Tiny muscles in the iris (coloured part of the eye) control how much light enters the pupil
- Sclera (white part of the eye): This tough covering protects the eye and gives it a firm shape
- Lens (clear crystalline curved structure behind the iris): This fine-tunes the light focused on the retina. Its shape changes so you can focus on objects at different distances
- Cornea (clear dome covering the front of the eye): This works with the lens to make sure light coming in focuses on the retina
- Retina: This light-sensitive layer converts light into electrical signals, which are sent to the brain and processed to create an image
- Macula (small area near the middle of the retina): This is responsible for central vision and the ability to see details
- Vitreous humour (clear jelly-like material): This fills the middle of the eye between the lens and retina
- Optic nerve: This carries electrical signals from the retina to the brain.
What can go wrong?
Many common visual problems start in childhood. People with long-sightedness (hyperopia) can see distant objects clearly but find it harder to focus on close objects. This occurs if the eyeball is shorter than it should be or if the cornea is too flat. People with short-sightedness (myopic) find it harder to see into the distance but close objects are clear. This may occur if the eyeball is too long or if the cornea is too curved. Astigmatism is a common cause of blurred vision – it occurs when the eyeball has an abnormal shape, usually more oval than round.
Adults often notice their close vision worsens from around the age of 40. Called presbyopia, this is normal but can cause eye strain or headaches if they don’t wear suitable reading glasses. Regular eye checks are important to rule out serious sight problems. Chronic conditions such as glaucoma and cataracts need to be treated early on to avoid permanent sight loss. Some common eye problems, such as eye infections, eye strain, dry eyes and blepharitis, may be treated in the pharmacy setting, but any changes in vision should be assessed by an optometrist.
“Chronic conditions need to be treated early on to avoid permanent sight loss”
Contact lens hygiene
According to the Royal National Institute of Blind People (RNIB), more than four million people in the UK wear contact lenses to correct their vision. Contact lens hygiene is essential to reduce the risk of an infection that could lead to serious eye damage. Useful hygiene tips for customers include:
- Always wash and dry hands thoroughly before handling contact lenses or touching the eyes
- Always use a contact lens solution to clean and disinfect reusable contact lenses – only use a solution recommended by the optometrist
- Never reuse old contact lens solution
- Don’t use tap water (or saliva) to clean or wet lenses as it isn’t sterile
- Never sleep while wearing contact lenses (unless approved by an optometrist)
- Don’t wear contact lenses for any longer than an optometrist has advised
- Never swim in contact lenses Never wear contact lenses if the eyes look red or feel sore or irritated.
Eye strain
Eye strain can occur when the eyes focus intensely on a particular task (especially a screen) without a break. It usually disappears after resting the eyes and doesn’t lead to permanent damage. Using eye drops and eye masks may help to ease tiredness and irritation.
“Eye sprays, applied to closed eyelids, can be useful for people who find conventional eye drops uncomfortable or challenging to use,” says Aishah Patel, clinical adviser at the Association of Optometrists. “These can be beneficial for mild dry eye symptoms and irritated eyes, especially those caused by environmental factors such as exposure to dry air, smoke or UV light.”
Conjunctivitis
Conjunctivitis (inflammation of the conjunctiva) can affect one or both eyes. Symptoms vary, depending on the cause.
“It can be difficult to tell viral conjunctivitis from bacterial conjunctivitis,” says Dr Elizabeth Hawkes, consultant ophthalmologist, oculoplastic surgeon and aesthetic doctor at: drelizabethhawkes.com. “Sometimes a clue to the diagnosis can come from the history – for example, viral conjunctivitis tends to result in a watery discharge, is often bilateral and associated with other upper respiratory tract infection signs (such as a running nose, sore throat and cough). Bacterial conjunctivitis on the other hand often has a purulent (yellow/green) discharge. A further challenge is that the above symptoms can often be seen with allergy.”
Conjunctivitis doesn’t always need any specific treatment, other than cleaning the eyelids with sterile pads and clean water. “Antibiotic eye drops are only appropriate for bacterial conjunctivitis, and they won’t treat viral conjunctivitis,” says Aishah. “Using a cold compress and taking a non-steroidal anti-inflammatory medicine, such as ibuprofen, can help improve comfort. If the infection doesn’t improve within two weeks, advice should be sought from an optometrist.”
Dry eye
According to Scope Eyecare, 44 per cent of the population report dry eye symptoms. Dry eye occurs when the eyes don’t make enough tears or if the tears are of poor quality. The eyes feel itchy and uncomfortable and may water regularly to compensate for the lack of tears. Blurred vision can be a problem, along with contact lens discomfort. Dry eye often affects people as they get older, especially women experiencing the menopause.
“We naturally blink less when looking at screens, so our eyes lose moisture. The quickest and easiest way to restore eye moisture is to use eye drops, while also making sure you stay properly hydrated,” says Mark Holloway, optician at Thomas & Holloway Opticians in Dronfield, speaking on behalf of TheraTears. “I also strongly recommend the 20-20-20 routine; every 20 minutes, look away from your screen for 20 seconds and focus on something 20 metres away to give your eyes a break and a chance to readjust.”
There’s some evidence that eating a diet rich in omega-3 fatty acids, or taking these as dietary supplements, can relieve dry eye. It’s also important to avoid smoky or air-conditioned environments as much as possible. Dry eye products from pharmacies include heated eye masks and preservative-free dry eye drops, gels or ointments.
“Eye drops are a good first-line option and [are] highly recommended for daytime use,” says Dr Hawkes. “Gels are more viscous and tend to be useful when the dry eye symptoms are more severe, because they give longer-lasting lubrication. We tend to give night ointments for use just before bed. Ointments can smear the vision for a few hours – not a problem if you’re asleep, but clearly not ideal when walking around in the day.”
Although dry eye can often be managed in the pharmacy, long-term symptoms should be assessed by an optometrist or GP. Possible causes of chronic dry eye syndrome include medical problems (such as diabetes, rheumatoid arthritis or Sjögren’s syndrome), taking certain medicines (such as antihistamines) or a blockage in the eyelid glands that make the oily layer of tears – called meibomian gland dysfunction (MGD).

Blepharitis
Blepharitis is more common in people over 40, causing itchy, sore or red eyes and crusty or greasy eyelashes and eyelids. It can be caused by an infection but may also be associated with seborrhoeic dermatitis or rosacea.
The best way to manage blepharitis symptoms is to wash the eyelids daily.
“Patients will need to use a cleansing product to remove all the debris from the edge of eyelids and between the eyelashes,” says Aishah. “Warm water and cotton balls may be an alternative for unclogging glands. In longstanding cases where eyelid wipes and gels have been ineffective, antibiotic ointment may be required. If symptoms persist or become worse, such as significant swelling, burning, soreness or a noticeable reduction in vision, it’s best to consult an optometrist.”
Glaucoma
Glaucoma is a group of eye conditions that damage the optic nerve. It’s often caused by high pressure inside the eye (intraocular pressure). Glaucoma doesn’t usually cause any symptoms, especially in the early stages, and is diagnosed during a routine eye check.
Chronic (primary open-angle) glaucoma is the most common type, usually developing gradually and without any pain. It affects around two in every 100 people over 40: risk factors include a family history of glaucoma, African-Caribbean ethnicity, diabetes and very high blood pressure. Acute (primary angle-closure) glaucoma happens very quickly due to a sudden rise in eye pressure and is a medical emergency. It may cause pain, blurred vision and haloes around lights, and can lead to sight loss if it’s not treated quickly.
Glaucoma can be treated with eye drops, laser treatment or surgery, depending on the type of glaucoma. The eye drops need to be used long-term or for life, and it’s important to use them as recommended. There are many different types, and it can take trial and error to find the right one or combination. An optometrist will provide tailored advice.
Cataracts
Cataracts occur when the lens inside the eye loses transparency so light can’t reach the back of the eye. These are more common as people get older. Risk factors include family history, smoking, heavy drinking and regular exposure to strong UV light. Cataracts usually develop slowly over several years, so most people don’t notice symptoms at first. Vision may eventually be blurred, misty or cloudy, colours may seem faded or have a yellow or brown tinge, and lights may seem too bright to look at. The only effective treatment is surgery.
“Cataract may be worse in one eye at first, but usually, with time, both eyes become affected, depending on the cause,” says Mr James Neffendorf, consultant ophthalmologist and vitreoretinal surgeon (mrjamesneffendorf.com). “Once the visual problems caused by cataract are affecting your life, it’s helpful to discuss your options with a cataract surgeon.”
Floaters
Floaters are very common and generally nothing to worry about. As people get older, the jelly-like vitreous humour in the eyes gets more watery and pulls away from the retina. This is called posterior vitreous detachment and it usually happens after the age of 50. It is not uncommon for it to go unnoticed for many people. Floaters may look like dots, strands, spiders or cobwebs, especially when looking at a plain background, such as a white wall or the sky. Eventually, they sink out of vision or the brain learns to ignore them. Wearing dark sunglasses outside can help to make them less noticeable.
If people have an increase in new floaters, especially with flashing or flickering lights, they should see an optometrist straightaway. This could be due to a retina tear or retinal detachment, which is an emergency requiring surgery.
“It’s recommended to be examined by a retina specialist within 24-48 hours if you develop a sudden onset of flashes and floaters,” says Mr Neffendorf. “Approximately five to 10 per cent of patients who develop a posterior vitreous detachment can have a retinal tear as a result of the pulling. This requires urgent laser or cryotherapy treatment to reduce the chance of a retinal detachment.”
Sight loss-friendly pharmacies
More than two million people are living with sight loss in the UK, notes the Royal National Institute of Blind People (RNIB). This can affect their ability to access pharmacy advice and use medicines correctly and safely. The Specialist Pharmacy Service website has information on helping people with sight loss manage their medicines:
- Use colour-contrasted lines on the pharmacy floor to help navigate people to the counter and consultation room. Make sure there are no obstacles, such as chairs, blocking the way
- Position signs at eye level so people can see them clearly. If someone approaches the pharmacy counter, state your professional role and how you can help them
- Call out names of people collecting prescriptions instead of (or as well as) using a visual display or number
- Use large-print labels (and larger labels). Labels with black bold text on a yellow background are easiest for people with sight impairment to read. The RNIB sells a braille labelling machine
- Mark medicine containers with different signs or colours to differentiate between them. Tie two rubber bands around medicines that need to be taken twice a day, or a long rubber band with three knots in it for medicines to be taken three times a day
- Send the customer an email with specific medicines advice and website links to online patient information leaflets.

