In Conditions
Follow this topic
Bookmark
Record learning outcomes
Asthma is an extremely common condition in the UK, affecting 7.2 million people, according to charity Asthma + Lung UK. The condition affects a person’s breathing, and as it currently does not have a cure, is a life-long affliction.
This makes it all the more important for people with asthma to know how to manage their condition, how to correctly take their medication, and understand when they may need to revisit their clinician. The consequence for not doing so can be fatal – a shocking outcome considering that good self-management practices and medication awareness can allow people to live long and healthy lives with the condition.
Why, then, does the UK have one of the highest asthma death rates in Europe, and what can pharmacy teams do to combat this?
“Four people in the UK die from an asthma attack every day”
The state of asthma care
“There has long been a need to do better for the 7.2 million people in the UK living with asthma. The UK continues to have one of the worst asthma death rates in Europe: asthma deaths have risen in the past decade and four people in the UK die from an asthma attack every day,” says Dr Andy Whittamore, clinical lead at Asthma + Lung UK.
The high asthma death rate in the UK is a reflection of the state of asthma care across the UK, where a lack of awareness partnered with the lack of access to quality care combine to create a perfect storm of inadequate asthma management.
“A recent survey by Asthma + Lung UK showed that, shockingly, seven out 10 people with asthma aren’t receiving the recommended basic care they need to stay well, which includes a personalised asthma action plan (PAAP), annual review and inhaler technique checks,” says Dr Whittamore.
“It is even worse for children, with less than a quarter receiving all three aspects of basic care. This collapse in care means people with asthma have less control over their condition, a higher risk of asthma attacks, and an increased risk of hospitalisation and death.”
What is asthma?
Asthma is a long-term lung condition which affects the breathing tubes (airways) that carry air in and out of the lungs by making them inflamed. As the airways swell, they become narrower, and less air can travel to and from the lungs.
“The exact cause is still poorly understood; however, it is seen as a genetic condition that is affected by environmental, maternal and early childhood factors,” says Dhiren Dayal, advanced clinical pharmacist and British Thoracic Society member.
“The diagnosis of asthma is defined by the history of respiratory symptoms, such as wheeze, shortness of breath, chest tightness and cough, that vary over time and in intensity, together with variable expiratory airflow limitation.”
Diagnosis
For some people, asthma is triggered by exercise, while for others, high levels of air pollution may bring on symptoms. Other triggers include cold air and/or encountering an allergen such as pollen, dust, mould, or animals.
Anyone exhibiting symptoms should book an appointment with their GP as soon as possible – if it is asthma, they should get treatment straight away.
The appointment usually consists of a discussion of symptoms, testing how the lungs are working, and the GP will also listen to the chest for any sounds of wheezing. There are then four main asthma tests that can confirm a diagnosis:
- A blood test which measures eosinophil levels (a type of white blood cell)
- Fractional exhaled nitric oxide (FeNO) tests which measures the amount of inflammation in the airways
- Spirometry tests which measure how much air someone can blow out in one forced breath
- Peak flow tests which measure how fast someone can blow air out of their lungs.
Some people may be given a peak flow meter to take readings themselves over a few weeks. If asthma is suspected, asthma treatments may be prescribed to see if they help – which if they do, may confirm the asthma diagnosis.
“Asthma is different for everyone who has it, and symptoms vary over time. Your GP or nurse will want to do tests and try out treatments before confirming a diagnosis of asthma,” says Asthma + Lung UK.
“For this reason, you may not get a confirmed diagnosis in your first appointment. It’s important that the diagnosis is thorough to make sure you get the correct treatment.”
“Seven out of 10 people with asthma aren’t receiving the recommended basic care they need to stay well”
Encouraging better self-management
If asthma is diagnosed, people should fill out an asthma action plan – a record of how to manage their asthma, and what to do if symptoms get worse – with their GP or nurse. This should be kept up-to-date and taken to asthma reviews which should occur yearly, even if the asthma is being well-managed.
Asthma medication is delivered through inhalers, so it is vital that when someone is diagnosed with asthma, they are taught how to use them correctly.
“It’s vital that we improve awareness of the seriousness of asthma. Healthcare professionals need to have the training, time and resources to understand each individual, ensuring they get all the recommended elements of basic care each year,” says Dr Whittamore.
This treatment pathway seems relatively straight forward; receive diagnosis, record symptoms, collect prescribed medication, inhalers – there are various types of inhalers, which are used slightly differently for different purposes – and self-administer.
But why are so many asthma sufferers in the UK unable to stick to this regimen? A recent article by Asthma + Lung UK called for a new approach to asthma self-management, citing that of the high number of asthma-related deaths in the UK, “over half of these are considered preventable through better self-management”.
Dr Whittamore believes that increased focus on individuals autonomously managing their asthma is crucial. “There must be a focus on supporting people to manage their condition themselves, [which includes recognising] when they need to seek help,” he explains.
“For example, when someone is using their blue reliever inhaler three or more times a week, it’s a sign of untreated inflammation in their airways and it’s really important for them to make an appointment with their GP, nurse or pharmacist to discuss treatment options. It shouldn’t get to the point where someone is rushed to hospital fighting for breath.”
Dr Whittamore implored anyone who feels like they need advice on any asthma related queries to make use of the Asthma + Lung UK helpline (0300 222 5800) or visit their website: asthmaandlung.org.uk.

Teaching children and their parents or guardians the correct way to use inhalers is crucial to ensuring the medicine is effective.
Your part to play
“Community pharmacy teams are well placed to play a key role in supporting people with new treatments, ensuring they are using their inhalers as prescribed and with the correct inhaler technique,” says Dr Whittamore.
Dhiren suggests that pharmacy teams can help by:
- “Identifying patients who may be overusing their Short-Acting Beta-2 Agonist (SABA) and signposting them to have an asthma review at their practice or liaising with the GP practice team to highlight this
- Supporting patients with their inhaler technique and ensuring they know how to use their inhalers
- Addressing adherence concerns the patient may have with their inhaled corticosteroids (ICS)
- Supporting patients to give up smoking by either enrolling them in smoking cessation programme or providing smoking cessation advise though the technique of Very Brief Advice [from the National Centre for Smoking Cessation and Training]
- Ensuring patients have their required vaccinations at appropriate times to reduce their risk of an asthma attack/exacerbation, e.g. seasonal influenza, pneumococcal, Covid-19 and respiratory syncytial virus (RSV)
- Supporting patients with their new inhalers using the New Medicine Service
- Ensuring patients discharged from hospital with new inhalers are supported through the Discharge Medicines Service
- Helping support patients to manage their hayfever effectively (e.g. non-sedating antihistamines and/or intranasal steroid spray) which can be an important trigger for their asthma, leading to worsening of their asthma control
- Supporting them with their general health and wellbeing by signposting them to appropriate mental health services if they are suffering from anxiety, or providing any weight management advise. Both anxiety and obesity are co-morbidities that can make the patient’s control of their asthma more challenging.”
Asthma + Lung UK have a plethora of resources available on their website, including for people working in healthcare.
In providing support for people with asthma, pharmacy teams can hopefully make a difference in the number of asthma-related fatalities in the UK.

Any cough that has persisted for three weeks should be referred, especially if the cough is accompanied by phlegm or blood.
Knowing pneumonia symptoms
Pneumonia is a serious condition of the lungs which develops after a viral, bacterial or fungal infection that inflames the air sacs in one or both lungs.
With prompt treatment, most people get better in two to four weeks. It can be fatal if it causes complications such as respiratory failure, sepsis, septic shock, organ failure and the worsening of existing medical conditions.
“Anyone who is immunosuppressed has a higher risk both of developing pneumonia and of becoming seriously ill when they do develop pneumonia,” says Jeremy Brown, professor of Respiratory Infection at University College London and Respiratory and Infection Lead at Breathing Matters, which includes COPD.
Pneumonia red flags include:
- A cough of green or yellow mucus
- Shortness of breath
- A high temperature
- Chest pain
- Aching body
- Feeling very tired
- Loss of appetite
- Wheezing noises when breathing – babies may make grunting noises
- Feeling confused (common in older people).
“In pneumonia, the patient will tend to have a higher fever, feel more ill and often get short of breath. Pneumonia can also sometimes cause pleurisy, which is a sharp chest pain on breathing in, usually occurring at one spot on the side of the chest,” says Jeremy.
Referrals should be especially urgent if the customer has had a cough for three weeks or more, they are coughing up blood, have chest pain that comes and goes or happens when breathing or coughing, and anyone feeling short of breath.
Under the COPD umbrella
Asthma + Lung UK break down the meaning of chronic obstructive pulmonary disease (COPD) by describing it like this:
- Chronic: a long-term condition that does not go away
- Obstructive: the airways are narrowed, making it harder to breathe out quickly, and air gets trapped in the chest
- Pulmonary: it affects the lungs
- Disease: it is a medical condition.
“Chronic bronchitis and emphysema are both forms of chronic obstructive pulmonary disease,” says Dhiren Dayal, advanced clinical pharmacist and British Thoracic Society member.
“Chronic bronchitis is an abnormality of the airways caused by overproduction and hypersecretion of mucus by goblet cells, which leads to worsening airflow obstruction.”
It is not caused by a virus or bacteria, but through environmental factors that affect the lungs like smoke, hence, it is extremely common among long-term smokers and those exposed to air pollution.
“The most obvious and important thing to help anyone with chronic bronchitis who is still smoking is to stop smoking; this now also means try to stop vaping as well,” says Jeremy Brown, professor of Respiratory Infection at University College London and Respiratory and Infection Lead at Breathing Matters.
Emphysema, meanwhile, is when the walls of the alveoli – millions of tiny air sacs which fill with air when you breathe in and empty when you breathe out – become damaged.
“They break apart and merge into each other, creating holes in your lung,” according to Asthma + Lung UK. The main symptom is shortness of breath, and there are different types of emphysema depending on where these holes have developed in the lung.
Pharmacy teams should similarly strongly encourage customers with emphysema to quit smoking, which will only continue to exacerbate the condition.
Customers will most likely be using bronchodilators, which relax the muscles in the airways daily to reduce swelling and mucus production in the aways. These look like inhalers and/or inhaled corticosteroids.
Remind customers collecting medication for their chronic bronchitis or emphysema that it is important for them to consistently follow their prescribed regime to avoid flare-ups.
They should also maintain a healthy weight through regular exercise, being advised not to push themselves too far.
The NHS suggests consulting a GP or participating in a pulmonary rehabilitation programme where a customised exercise plan can be created.
Getting vaccinated is also extremely important for anyone with COPD, so remind customers when vaccination programmes are available.
Lastly, ensure customers keep an eye on the weather, as cold spells and periods of hot weather can cause breathing problems; ensure that they have medication on hand in case of flare-ups.
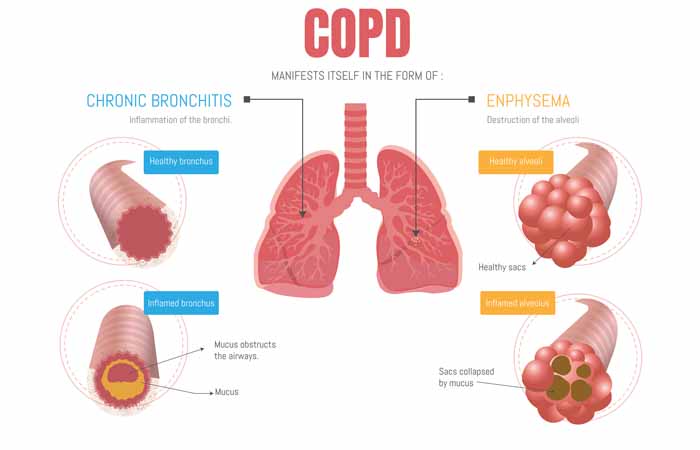
Chronic bronchitis and emphysema are both forms of chronic obstructive pulmonary disease (COPD).