There are more than 18,000 care homes providing care to approximately 460,000 adults and older people in England. There are two types of care home for adults:
- 'Care homes without nursing' provide personal care only (e.g. help with washing, dressing, eating and giving medicines)
- 'Care homes with nursing' (CHN) have a qualified nurse on duty 24 hours a day to carry out nursing tasks in addition to these personal care tasks, but some may accept people with personal care needs who may need nursing care in the future.
The most common conditions experienced by people in care homes are dementia, stroke, degenerative neurological conditions, advanced cardio-respiratory disease, cancer and painful arthritis.
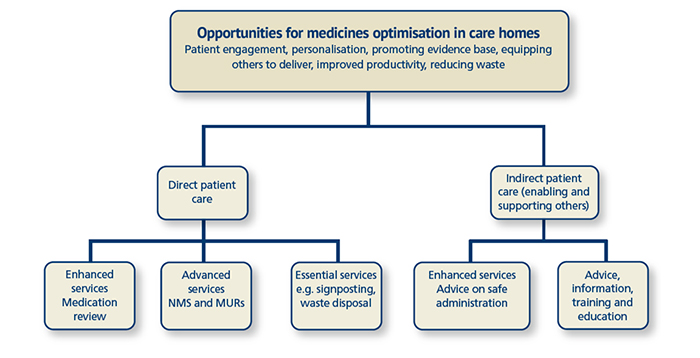
Historically, regulation, guidance and national standards focused on care homes having policies and procedures in place to ensure safe medicines management. More recently, the emphasis has shifted to medicines optimisation, which is a patient outcome-focused approach to safe and effective use of medicines that takes into account the patient's values, perception and experience of taking medicines.
Key issues
Age-related physiological changes that affect drug handling, polypharmacy and multiple morbidities increase the risk of adverse drug events (ADEs) and make prescribing in older people more challenging. Reduced functionality, frailty and cognitive deficits accompanied by poor eating and drinking add to this challenge. Care home residents also move across care settings and are at a higher risk of drug errors and ADEs.
Polypharmacy, in particular, is a key concern. Care home residents take an average of eight medicines and the incidence of ADEs increases with the number of drugs taken. Polypharmacy is also associated with non-adherence, drug-drug interactions, wastage, hospital admissions and increased workload.
The Care Homes' Use of Medicines (CHUM) study found that residents have a 70 per cent chance of experiencing a medication error, with many errors being related to poor communication between the care home, dispensing pharmacy, GP practice and secondary care.
