After discharge from hospital, problems with medicines include the risk of unintended medicine changes, unintended non-adherence and the possibility of adverse drug reactions, which may result in poorer outcomes including readmission to hospital.
During a stay in hospital, a patient's medicines may be changed, and a report by the Care Quality Commission (CQC) in 2009 highlighted that almost half of all patients may experience an error with their medicines after they have been discharged. The transfer of patients and their medicines from secondary care to primary care and vice versa can lead to:
- Incorrect transmission of information
- Unintended changes in medication
- Intended changes in medication not being followed through (e.g. changes in medicine, dose or formulation)
- Continuation of medication that should have been discontinued.
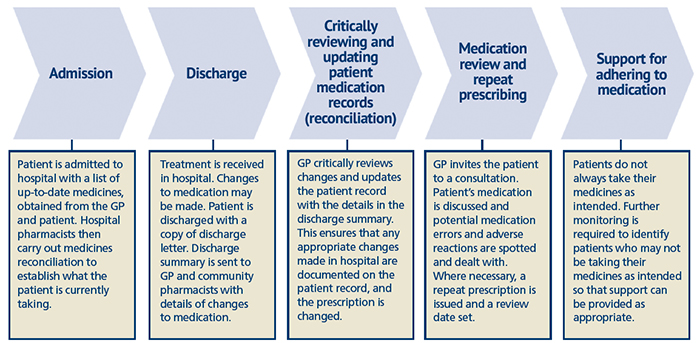
Community pharmacists can use both MURs and the NMS, as well as information from hospital colleagues, to improve patient care. Figure 1 (below) from the CQC's 2009 report shows the steps that need to be in place to ensure that medicines are obtained and used by patients as intended after discharge from hospital, and the ideal patient pathway in relation to this. Community pharmacy can contribute to the final stage of this pathway ('support for adhering to medication') through MURs.