In In-depth
Follow this topic
Bookmark
Record learning outcomes
Antimicrobial resistance (AMR) remains one of the top global public health threats facing humanity and was associated with the death of close to five million people globally in 2019, according to the World Health Organization (WHO).
In response, WHO has published its first global research agenda for the world’s scientists to address the most urgent human health priorities to combat AMR. It outlines 40 research topics on drug-resistant bacteria, fungi and Mycobacterium tuberculosis that must be answered by 2030, in line with the Sustainable Development Goals in order to spur on innovation and implementation research to prevent infections and emergence of resistance.
This comes hot on the heels of the UN Environment Programme’s February 2023 report – Bracing for Superbugs: Strengthening environmental action in the One Health response to antimicrobial resistance – which considers how using the ‘One Health’ approach to recognise that the health of people, animals, plants and the environment are closely linked and interdependent is vital in order to address the threat of up to 10 million deaths per year caused by AMR forecast by 2050.
What is AMR?
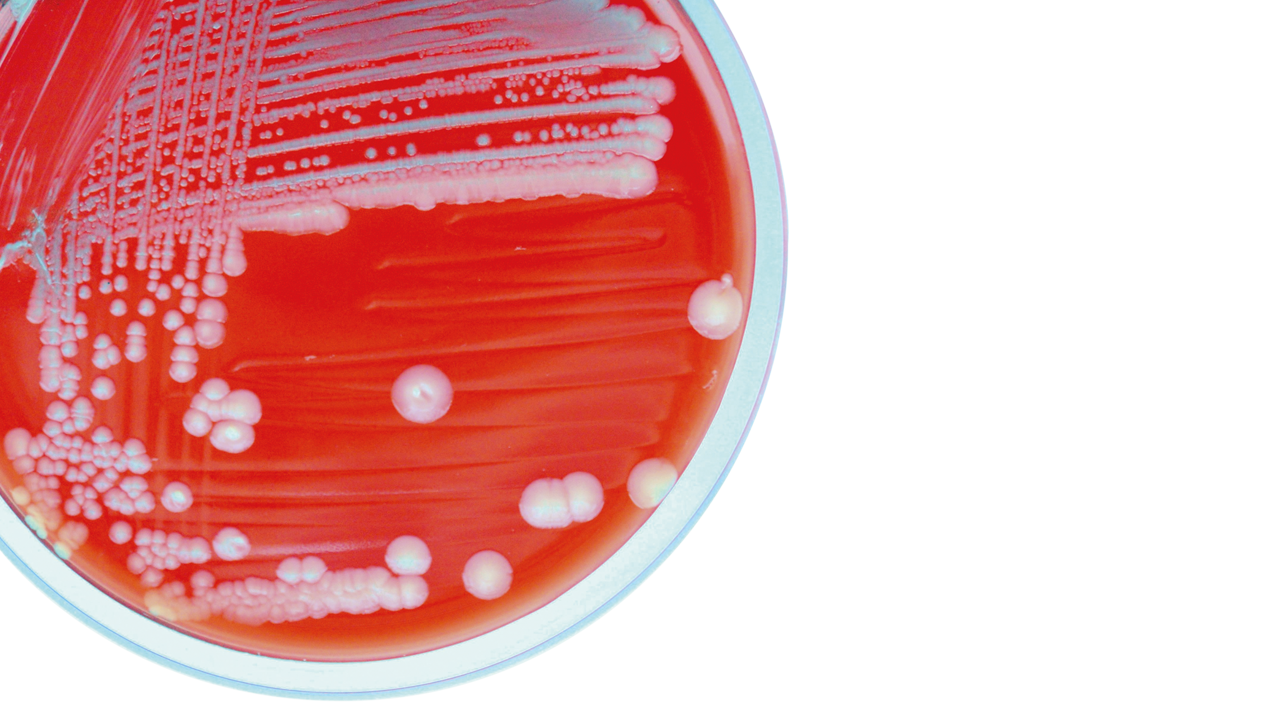
AMR occurs when bacteria, viruses, fungi and parasites change over time and no longer respond to antimicrobial medicines, making infections harder to treat and increasing the risk of disease spread, severe illness and death.
As a result, antimicrobial medicines become ineffective and infections persist in the body, increasing the risk of transmission to others. Global attention to AMR has mainly focused on the increased use and misuse of antimicrobials in the human health and agriculture sectors, but there is growing evidence that the environment plays a key role in the development, transmission and spread
of AMR.
According to the UN’s report, other microbial stressors such as pollution create favourable conditions for microorganisms to develop resistance both in humans and the environment from sources such as sewage, and bacteria in water, soil and air can then acquire resistance following contact with resistant microorganisms.
The report notes that environmental dimensions of AMR include pollution from hospital and community wastewater, effluent from pharmaceutical production, run-off originating from plant and animal agriculture and other forms of waste and releases. These may contain not only resistant microorganisms, but also antimicrobials, various pharmaceuticals, microplastics, metals and other chemicals, which all increase the risk of AMR in the environment – a risk which the UN says is increasing.
In addition, the key economic sectors contributing to the environmental dimensions of AMR include pharmaceutical and other chemical manufacturing, as well as healthcare delivery in hospitals, medical facilities, community healthcare facilities and in pharmacies where a broad range of chemicals and disinfectants may be used.
On a positive note, the report says there is enough knowledge to implement measures to reduce the factors that influence AMR from an environmental perspective, which will also address “the triple planetary crisis by addressing sources, sinks and waste”.
The solution, says the UN, is to use the ‘One Health’ approach to address AMR, with the report noting some countries have already adopted this approach into their National Action Plans on AMR, alongside voluntary industry initiatives establishing common framework for managing discharge of antimicrobial compounds, and international organisations launching initiatives such as the joint efforts of the Quadripartite Alliance (FAO, UNEP, WHO and WOAH) for strong and coordinated action.
Yet still more needs to be done to address “biological wastes that contain resistant microorganisms that spread AMR, and chemical wastes that select for AMR”. The report calls for priority action to address key pollution sources from poor sanitation; sewage; community and municipal wastes; healthcare delivery; pharmaceutical manufacturing; intensive crop; and terrestrial and aquatic animal production sectors.
Noting that “prevention is at the core of the action and environment is a key part of the solution”, the UN says there are “numerous stakeholders” at national, regional and international levels to take forward actions to tackle AMR in the environment, including community groups, youth, consumers’ associations, professional organisations and schools for professionals including pharmacists, veterinarians and farmers.
Spotting sepsis
While it is important to prevent the emergence of antimicrobial resistance by limiting antibiotic use, it is vital to be aware of life-threatening conditions such as sepsis – a common and potentially life-threatening state triggered by an infection.
Warning symptoms that require urgent medical attention include:
- Slurred speech
- Extreme shivering or muscle pain
- Passing no urine (in a day)
- Severe breathlessness
- Mottled or discoloured skin.
Action now
All healthcare workers have a role in tackling antimicrobial resistance, and pharmacy teams are well placed to make sure customers understand why AMR is such a threat.
“Antibiotics have significantly reduced deaths from common infections. For example, less than one in 100 young and otherwise healthy people now die from community-acquired pneumonia and skin infections in comparison to the 10 in 100 people who died before antibiotic use,” says Professor Diane Ashiru-Oredope, lead pharmacist, HCAI, Fungal, AMR, AMU & Sepsis Division, UK Health Security Agency. “If antibiotics are lost, society risks returning to the days when those infections now regarded as trivial become fatal again. An infected cut could be life-threatening and an illness like pneumonia would again become a mass killer.”
A role for pharmacy
Since community pharmacies are at the frontline of appropriate medicines management and supply, staff can also explain to customers why everyone has a role to play in the ‘One Health’ approach to address AMR.
A good place to start is with the importance of hygiene in reducing infection risk. “Preventing infections will play a major part in tackling antimicrobial resistance because it reduces the need for antibiotics in the first place”, says Diane, “and hand hygiene is also important in preventing transmission of infection in all health and social settings. Cleaning hands properly is the single most important thing anyone can do to help reduce the spread of infections. Hands should always be washed with soap and water if they are visibly soiled or after using the toilet. Alcohol handrub can be used if hands are visibly clean but is not effective against some infections (e.g., Clostridium difficile).”
Vaccination and resistance is another area to focus on – for example WHO estimates that flu causes about 250,000-500,000 deaths annually worldwide.
“Providing a vaccine service or signposting at-risk patients to other relevant services where they can receive their vaccination is another important public health action that can help stem the rise of antimicrobial resistance,” adds Diane. “Vaccines can decrease the use of antibiotics directly by preventing primary infection and indirectly by preventing bacterial superinfection after a primary vaccine-preventable illness, such as influenza.”
Community pharmacy teams are also ideally placed to provide effective self-care advice for patients with self-limiting infections – especially since, according to Diane, “previous studies have shown that one-third of the public believe that antibiotics will treat coughs and colds, and one in five people expect antibiotics when they visit their doctor”.
“Pharmacy teams are familiar faces to many people who use their community pharmacy and trusted sources of help and information”, says Mark Gilchrist, chair of the RPS Antimicrobial Expert Advisory Group, “and their advice on self-care and over-the-counter medications helps promote appropriate management of minor ailments and reduces the unnecessary use of antibiotics”.
Similarly, pharmacy staff play an important role when providing prescribed antibiotics in relaying information about completing the course, and to not share antibiotics with anyone else. “Staff can engage with patients to ensure these messages are understood and land well with individuals, as they often know patients well and can tailor their approach accordingly,” adds Mark.

Cleaning hands properly is the single most important thing anyone can do to help reduce the spread of infections.
Self-care advice
Alongside appropriate medicines use, pharmacy teams are also the experts on self-care advice to help with conditions, such as:
- Getting plenty of rest
- Drinking enough fluids to stay hydrated
- Taking paracetamol or ibuprofen for pain relief or to relieve a fever.
Pharmacy staff should also be confident in recognising and advising customers on ‘red flags’ which indicate when to refer to their GP, such as:
- Persistent raised temperature (39°C and above) for longer than three days
- Severe headache with vomiting or severe earache
- Coughing blood/blood-stained mucus on more than one occasion
- Chest pain
- Difficulty in breathing
- Difficulty in swallowing
- Unusual skin rash
- Confusion, slurred speech, drowsiness.
Getting the message across
Pharmacy teams can also be the drivers who actively engage in public health campaigns and initiatives to raise awareness about AMR and the importance of responsible antibiotic use.
Posters, leaflets, quizzes and videos to educate the public, other pharmacy staff and healthcare professionals are available through national campaigns in the UK.
European Antibiotic Awareness Day (EAAD) is an initiative held each year on 18 November, while WHO launched World Antibiotic Awareness Week to run during the same week. Active promotion of EAAD is one of the key strategies listed by the Department of Health as being important in the UK five-year antimicrobial resistance strategy. Educational materials and resources that can be used as part of a health promotion campaign are available at: gov.uk, simply search ‘EAAD’ and click on ‘Antibiotic Awareness: toolkit’ 2022.
Finally, launched in 2014 to galvanise collective action from health and social care professionals as well as members of the public to work together to slow the spread of antibiotic resistance, the whole pharmacy team can become Antibiotic Guardians by pledging to contribute to antimicrobial stewardship efforts within community pharmacy.
Although many people have grown up asking healthcare professionals for antibiotics ‘just in case’ this is no longer the right approach, and pharmacy teams are in the ideal position to explain the real cost of using antibiotics when they are not needed – a price we now know is just too high to pay.
Further resources
The TARGET Antibiotic Checklist is part of the national Antimicrobial Stewardship resources for primary care and aims to support interaction between community pharmacy teams and patients prescribed antibiotics. The Checklist, completed by the pharmacy staff with patients, invites patients to report on their infection, risk factors, allergies, and knowledge of antibiotics.
- Find out more via the TARGET Antibiotics Toolkit of free resources and training
- Antibiotic awareness: posters and leaflets
- Short e-learning sessions on AMR.
Further resources:
- Anyone with an interest in the menopause, midlife and post-menopausal health can receive The Menopause Exchange quarterly newsletter for free
- A.Vogel Menopause Hub
- Women’s Health Concern menopause advice hub offers evidence-based, peer reviewed information to women and their partners.