In In-depth
Follow this topic
Bookmark
Record learning outcomes
It might sound strange to say that people are often at risk of poisoning themselves, but it occurs more often than many might think.
Accidental poisoning can happen after something as simple as taking paracetamol-containing cold and flu remedies too closely together, or, by not realising that weight loss surgery can alter the way the body absorbs medicines.
So, perhaps it’s not surprising to hear that poisoning causes a quarter of accidental deaths in the UK.
According to the Royal Society for the Prevention of Accidents, in 2022, 21,336 people across the UK died accidentally – a 42 per cent rise since 2013.
Falls accounted for 46 per cent of accidental deaths, but poisonings accounted for 26 per cent. Alarmingly, accidental deaths from poisoning roughly doubled (up 96 per cent) between 2013 and 2022.
But how can the pharmacy team help prevent accidental poisonings? The good news is that there is lots that pharmacy teams can do.
Methanol poisoning
If you know a customer is going to be travelling abroad, you can remind them to be careful when ordering alcoholic drinks.
Recently, drinks contaminated with methanol have caused serious illnesses and deaths in destinations as far apart as Japan, Mexico, Thailand, Turkey, Nigeria, Peru and Russia.
Because of this, the Foreign, Commonwealth & Development Office (FCDO) advises holidaymakers and other travellers to watch for signs of methanol poisoning and it urges caution when buying drinks.
To cut costs, some unscrupulous bars or drinks manufacturers mix methanol, which can be found in things like methylated spirits, antifreeze and paint thinners, with alcohol-based drinks and cocktails.
Methanol is tasteless and odourless, so it is easy for it to go unnoticed. Unfortunately, without treatment, as little as 25 to 90ml can be fatal.
The FCDO therefore advises buying sealed or bottled drinks from licensed premises, avoiding streetside or homemade alcohol, and being especially cautious of pre-mixed spirits, cocktails and drinks served in buckets or jugs.
At first, methanol poisoning can cause nausea, vomiting, dizziness, confusion, poor judgement, loss of balance, dizziness and drowsiness.
These early symptoms resemble alcohol poisoning, but more distinctive symptoms typically develop between 12 and 48 hours after consumption.
Symptoms of methanol poisoning include blurred vision, trouble looking at bright lights, “snowfield” (seeing snowy static), tunnel vision, and even complete blindness.
Other late symptoms include abdominal pain, vertigo, convulsions, difficulty breathing and coma.
Urgent treatment can reduce the risk of complications and even save lives, so anyone showing symptoms that may indicate methanol poisoning should seek immediate medical attention.
“Methanol poisoning can kill. It can be difficult to detect when drinking, and early symptoms mirror ordinary alcohol poisoning,” says Hamish Falconer, parliamentary under-secretary of state at the FCDO.
“By the time travellers realise the danger, it can be too late. I encourage all travellers to check our travel advice and Travel Aware pages [see Resources box, page 7] before they go on holiday.”
People also need to watch out for counterfeit and contaminated spirits closer to home. For example, in 2024, the Food Standards Agency (FSA) warned that counterfeit vodka on sale in the UK contained the industrial solvent isopropyl alcohol, which can cause nausea, vomiting, abdominal pain, intoxication, respiratory depression, cardiovascular collapse, coma and, in severe cases, death.
The FSA notes that “anyone with symptoms should seek medical attention” and that “the counterfeit vodka may have a strange smell and taste differently to genuine vodka”.

Customers should stick to bottled drinks when travelling to countries where methanol poisoning has occurred.
OTC overdoses
The National Poisons Information Service (NPIS) offers 24-hour, 365 days a year assistance to healthcare workers about diagnosing and managing poisoning.
Records of telephone enquiries to the NPIS in 2023 to 2024 offer a snapshot of poisoning in the UK. Thankfully, nine out of ten potentially poisoned patients experienced no symptoms or minor symptoms – but one in 1,000 people died.
As every parent knows, children tend to put anything in their mouths. This goes some way to explaining why, according to the NPIS, poisonings were most common in patients aged five years or younger (20.7 per cent of poisoned patients).
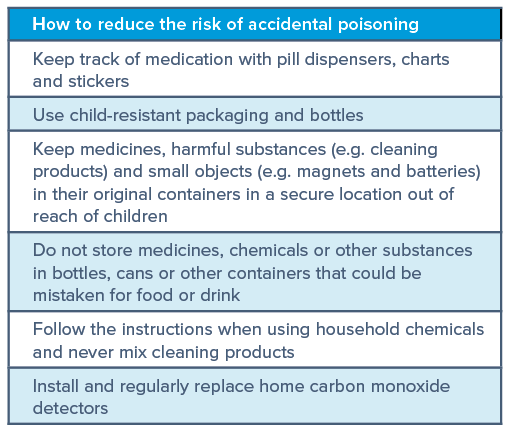
Taking simple precautions to stop children accessing potential poisons can make a big difference here (see table, above right).
The NPIS added that most poisonings were unintentional (37.7 per cent), by ingestion (88.3 per cent) and occurred at home (85.4 per cent).
Again, simple precautionary steps can help here. For instance, for people with cognitive impairment or dementia, medication dispensers, charts and stickers can help them to remember to take their medication at the correct time and avoid unintentional overdoses.
Sometimes the dose of a drug that treats a disease is close to, or even overlaps with, the amount that can cause serious side-effects. You may hear this referred to as a “narrow therapeutic window”.
People’s susceptibility varies and sometimes OTC medicines, prescription drugs and herbal remedies can lead to accidental poisonings.
Of course, not all poisonings are accidental. NPIS data show that almost one in four poisonings (22.8 per cent) resulted from deliberate self-harm, one in six were as a result of medication errors and one in 11 were caused by deliberately taking too much of a drug for therapeutic reasons.
It is important for pharmacy teams to watch out for people who may be at risk of self-harm, and also to remind all patients to follow the instructions when taking prescription as well as OTC medicines.
Knowing your pills
Just 10 to 15g of paracetamol can be lethal: that’s only 20 to 30 500mg tablets.
Some people accidentally overdose by taking different paracetamol-containing medicines, such as cold and flu remedies, too closely together.
The pharmacy team should remind people to always read the label and advise them to seek medical help if they experience symptoms of acute liver failure caused by a paracetamol overdose.
These include abdominal pain, irritability, clumsiness/poor coordination, fatigue, low blood sugar, jaundice, nausea and vomiting, sweating and trembling.
In general, adults can take two 500mg paracetamol tablets four times in any 24 hours. Remind customers that they must always wait four hours between doses and not take more than eight tablets in 24 hours.
People who weigh less than 50kg or who have liver disease should talk to a doctor or pharmacist about how much paracetamol they can take safely or whether they should use a different painkiller.
Children’s dosages should always follow the product packaging instructions, so familiarise yourself with these and remind customers that dosage is different for children of different ages.
Remember to be cautious about alternative remedies too. Just because a treatment is ‘natural’, ‘herbal’ or ‘derived from plants’ does not necessarily mean it is ‘safe’, warns the Medicines and Healthcare products Regulatory Agency (MHRA).
Some herbal products can cause serious side-effects, including liver damage. Certain natural products can interact with prescription and OTC medicines.
For example, St John’s Wort can reduce the effectiveness of the contraceptive pill, leading to unintentional pregnancy.
Some traditional medicines contain heavy metals and other toxic chemicals, including arsenic or mercury, as active ingredients, while contamination with substances like pesticides, fungal toxins and bacteria can occur during manufacturing.
In the past, traditional healers often started using poisonous chemicals to treat health conditions before they knew the risks. As recently as the early 20th century, for instance, physicians in the UK were still using mercury to treat syphilis.
Today, disreputable manufacturers may deliberately adulterate some herbal remedies with potent conventional medicines, such as sildenafil in herbal treatments for erectile dysfunction.
In some cases, the manufacturer adulterates the herbal product with a chemical relative (called an analogue) of a conventional medicine. The analogue may be more dangerous than the parent molecule or have unknown toxicity.
Having said this, herbal remedies are popular and many people do benefit from taking them. The best advice for customers is to use licensed herbal remedies from a reputable supplier or a qualified medical herbalist.
Weight loss surgery
Bariatric (weight loss) surgery reduces weight by reshaping the gastrointestinal tract. Indeed, it can reduce the size of the stomach by 70 to 80 per cent, so that the patient eats less. However, the changes can alter absorption of oral medications, leading to poor efficacy or side-effects and occasionally even contributing to fatal overdoses.
A study published in the British Journal of Clinical Pharmacology identified 18 people who had undergone bariatric surgery in the National Programme of Substance Use Mortality between 1997 and March 2025.
Twelve of these people had died from accidental overdoses, and prescription opioids had contributed to the deaths of all 17 of the people who had received them.
Potential poisons are everywhere: in our kitchen cupboards, medicine cabinets and, if we’re not careful, in our holiday libations. T
he pharmacy team can offer advice and support to help reduce the risk of accidental poisoning, including educating customers about the symptoms that may indicate poisoning and why, along with their sunscreen, they should pack a cautious approach to holiday drinking.
Resources
- British Liver Trust – Paracetamol overdose and your liver: britishlivertrust.org.uk/information-and-support/liver-conditions/paracetamol-overdose/
- JAMA – patient page: jamanetwork.com/journals/jama/fullarticle/2826704
- National Poisons Information Service: npis.org/
- MHRA and NHS Scotland – Information about herbal medicines: yccscotland.scot.nhs.uk/wp-content/uploads/2020/03/A4Herbalinformationleafletv9.pdf
- Royal Society for the Prevention of Accidents: rospa.com
- Travel Aware: travelaware.campaign.gov.uk