In Conditions
Follow this topic
Bookmark
Record learning outcomes
From constipation to cystitis, virtually all of us will experience bowel or bladder problems at some stage. And yet, even though these conditions are common, they can be some of the ones patients find hardest to talk about.
“We understand that many people experience feelings of worry or embarrassment when it comes to digestive symptoms and, as a nation, we’re still not comfortable talking about our guts,” says Julie Thompson, information manager at Guts UK (gutscharity.org.uk). “Digestive symptoms are very common and nothing to be ashamed about.”
Normalising conversations
Julie suggests that pharmacy teams can help by offering patients a private space in which to discuss concerns, providing information in accessible formats: “Promoting digestive health in your pharmacy through printed materials and posters or digital displays might help to reduce the stigma often associated with our guts.”
She also recommends that people get to “know your normal” by checking their poo, so that they’re then alert to any changes. “Guts UK’s Poo-Torial is a free online tool that helps you better understand the colour, consistency and frequency of your poo.”
Many bowel and bladder complaints can often be managed with self care measures and/or products from the pharmacy (always consider the patient’s age and any contraindications, and remind the customer to read the patient information leaflet). Even if further medical attention is needed, the sooner it can be sought out, the better.
Here, we take a closer look at some conditions pharmacy staff might encounter.
“Around 14 million people in the UK are living with incontinence problems”
Cystitis
Anyone who has ever suffered from cystitis – and around half of women will experience a bout at some point – knows the misery it can cause. Symptoms can include a stinging sensation while urinating, abdominal discomfort, and the urge to pass water more often – while younger children might also wet themselves, lose their appetite or seem generally irritable.
Cystitis is usually caused by a bacterial infection, leading to inflammation of the bladder. In some mild cases, it can clear up on its own, and patients may wish to take a suitable painkiller (such as paracetamol) in the meantime. However, other cases may need to be treated with antibiotics.
While patients traditionally needed to obtain a prescription from their GP, uncomplicated urinary tract infections in women aged 16-64 are now among the seven conditions covered under the Pharmacy First scheme, which launched in England in 2024.
If the patient meets the eligibility criteria, a participating pharmacist can assess them following a defined clinical pathway, and if appropriate, supply a restricted set of prescription only medicine.
While this option won’t be suitable for everyone (patients who should be referred to their GP include, among others, men, pregnant/breastfeeding women, those outside the 16-64 age range, people with a fever, and catheter wearers), it does mean many can seek treatment more quickly.
The NHS website says patients should see a doctor if symptoms are severe, occur frequently, or have not gone away within three days or after taking antibiotics; they should ask for an urgent appointment if they have a high or low temperature; nausea or vomiting; confusion or drowsiness; pain in their lower stomach or back; have not been able to pass water all day, or have blood in their urine.
If patients are prone to cystitis, and have seen their GP, some simple lifestyle steps may help to reduce bouts.
These include drinking plenty of water (and cutting down on alcohol/coffee), wiping from front to back when using the toilet, and trying to urinate shortly after sexual intercourse.
Incontinence
It’s estimated that around 14 million people in the UK are living with continence problems, though it’s hard to pinpoint a precise number, since many suffer in silence.
Though a common misconception is that it only happens to pensioners and new mums, it can affect anyone of any age and gender (though it is more prevalent in women).
There are several types of urinary incontinence, including:
- Stress incontinence: caused by pressure on the bladder
- Urge incontinence: when the patient suddenly feels the urge to go and can’t control it
- Functional incontinence: if a mental/physical condition prevents the patient getting to the toilet in time
- Overflow incontinence: when the bladder gets too full and leaks
- Mixed urinary incontinence: a combination of urge and stress incontinence.
Patients should see their GP in the first instance. Pharmacy staff can offer further support by signposting to relevant organisations, such as Bladder Health UK (bladderhealthuk.org), and being knowledgeable about the range of products in store, such as pads, incontinence pants, Radar keys and cleansing wipes.
Teams can also share advice on the benefits of pelvic floor exercises, maintaining a healthy weight, and smoking cessation (nicotine can irritate the bladder).
While patients might feel tempted to reduce their fluid intake, it’s important that they stay hydrated. Otherwise, urine can become more concentrated, which can make things worse. However, patients should try to cut down on alcohol and caffeinated drinks, which can have an irritating effect.

Help for haemorrhoids
Also known as piles, these are swollen blood vessels in and around the anus. In some cases, people might not know they have them, and they may clear up without treatment. However, other patients may spot symptoms such as bleeding after defecating (typically bright red), lumps or itching around the anus, or a mucus discharge.
“Rectal bleeding is a common symptom that can be caused by many conditions like haemorrhoids, fissures and polyps,” says Bowel Cancer UK’s (bowelcanceruk.org.uk) Claire Coughlan. However, as it can also be a sign of bowel cancer, the charity advises that patients should still see their GP.
If it is piles, there are products available from the pharmacy in a range of formats, including suppositories, creams, gels and ointments – as well as treatments to ease constipation and soften stools. However, the NHS advises against taking ibuprofen if piles are bleeding.
Patients should follow the treatment instructions but, as a guide, they should see their doctor if there is no improvement after a week, or piles keep occurring.
Liz from Warwickshire saw her GP when she began suffering from haemorrhoids after having three children. “I got it checked out because I was losing blood,” she says. “The doctor thought it was piles, but to be on the safe side I had a colonoscopy.
“In the end I had a band fitted, which cuts off the blood supply to the piles, then a couple of years later I had some more done. It was a simple procedure – a little uncomfortable afterwards at first, but I could manage it with paracetamol, and I was also advised to eat a high-fibre diet.” Other self care tips include drinking plenty of fluids, exercising, and wiping gently after going to the toilet.
If a patient has piles with pus, or a high temperature, they should see a doctor urgently; if suffering from severe pain or heavy blood loss, they should be referred to A&E.
Constipation
This can occur when bowel movements become infrequent (typically less than three a week) and/or stools are hard, dry and difficult to pass. It’s commonly caused by lifestyle factors, such as diet, but can sometimes also be a side effect of medication.
In many cases, it can be improved with some simple lifestyle changes, such as gradually increasing fibre intake, for example, by eating vegetables, fruit, brown bread and rice, pulses and higher-fibre breakfast cereals, drinking plenty of fluids, and taking regular exercise.
Laxatives are available from the pharmacy in a range of formats, including tablets, liquids and fibre drink sachets, but should be used short-term, paying attention to any instructions and restrictions, for example, they may not be suitable for young children or patients with Crohn’s disease.
If the problem persists, occurs regularly, involves stomach pain, it could be a side effect of medication, or the patient is showing signs of bowel cancer (see boxout), in which case they should see their GP.
“Up to 20 per cent of the UK population could have irritable bowel syndrome”
Diarrhoea
Whether caused by food poisoning, a virus, food intolerance, or anxiety, this common condition affects practically everyone at some point. Most cases are thankfully short-lived and can be self-managed with rest and rehydration (sticking to water or squash, and avoiding fizzy drinks/fruit juices).
Some patients may find an oral rehydration powder mixed with water helpful. An anti-diarrhoeal medicine such as loperamide can also be purchased without a prescription for patients aged 12 and up with short-term diarrhoea.
To reduce the risk of spreading an infection, patients should avoid preparing food for others if possible, and stay away from school, work and swimming pools until symptoms have stopped for at least 48 hours.
It’s also a good idea to wash hands often, clean high-contact surfaces regularly, and put any soiled laundry in a hot wash.
In more complex cases, people should call 111 or see a doctor – for example, if they’re concerned about a baby or child, are showing signs of dehydration, have bloody diarrhoea, or the problem persists for more than a week (or two days with vomiting).
Meanwhile, patients should call 999 or ask someone to take them to hospital in an emergency, such as if they develop sudden and severe stomach pain or headache, are struggling to breathe, or may have consumed something toxic.
Irritable bowel syndrome
It’s estimated that up to 20 per cent of the UK population could have irritable bowel syndrome (IBS), though the exact figures are hard to determine, as many people with symptoms may not be formally diagnosed. Signs of IBS include abdominal pain, wind, bloating, diarrhoea and/or constipation, and mucus in stools.
According to Julie, lifestyle measures that may help include avoiding aggravating foods, (for example, foods that are spicy and or fatty), limiting caffeine and alcohol intake, doing regular exercise, eating small portions slowly to minimise bloating, and keeping a food diary to spot triggers.
She also mentions “reducing dietary fibre to improve symptoms of diarrhoea or introducing a soluble fibre supplement to help constipation”.
Meanwhile, continues Julie, medicines and supplements available from the pharmacy might include probiotic supplements for up to 12 weeks; loperamide or intestinal adsorbents (to treat diarrhoea) or laxatives (to treat constipation), and OTC medications to reduce bowel spasms, such as peppermint oil capsules.
“Note that peppermint oil may make symptoms of reflux worse if someone has both conditions,” she adds.
If patients suspect they may have IBS, they should see their GP for further investigation.
Could it be cancer?
“Recognising the symptoms of bowel cancer is important for health professionals and the general population to help diagnose it as early as possible,” says Claire Coughlan, clinical lead for Bowel Cancer UK – adding that almost everyone survives if the disease is diagnosed at the earliest stage.
However, it is currently the second biggest cancer killer in the UK.
While those over 50 are at higher risk, patients can be affected at any age. “Changes in bowel habits – such as diarrhoea, constipation and the frequency of toilet visits – can be symptoms of bowel cancer if they last for three weeks or more,” explains Claire.
Other potential warning signs can include blood in poo, unexplained weight loss, abdominal pain, fatigue and iron deficiency anaemia. However, not everyone with the disease will have one of the more common symptoms – and some may not even have any. “This can make a diagnosis challenging,” she says.
There are steps that people can take to lower their likelihood of developing bowel cancer, she continues: “Keeping a healthy diet and staying active are some of the easiest lifestyle changes people can make to reduce their risk.”
On the other hand, “too little fibre in the diet, eating processed meat, being overweight or obese, drinking and smoking can all increase your risk”.
Pharmacy staff can play a vital role in raising awareness. “Proactively talking to the public, and the advice of pharmacy teams, can really help people to make an informed choice and drive forward informed participation in bowel screening,” Claire says.
“No screening test is 100 per cent accurate, so staying aware of symptoms is important. Even if a person has recently done a screening test, it’s important to speak to a GP if they notice any [symptoms].”
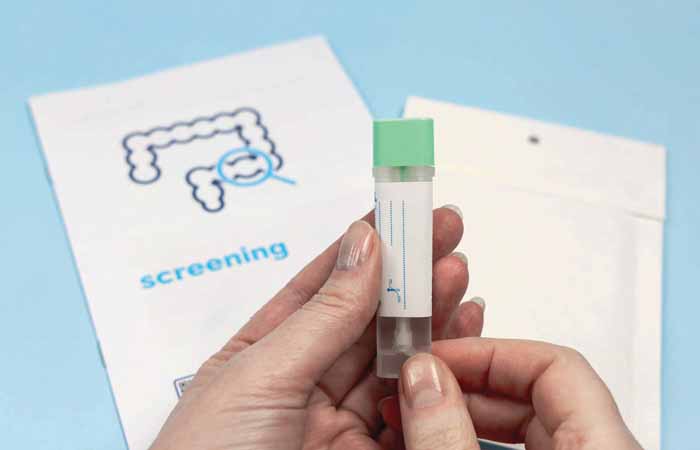
Customers should automatically be sent a free, at-home bowel cancer testing kit when they turn 50, but remind anyone concerned about symptoms to visit their GP to get checked.

