In Conditions
Follow this topic
Bookmark
Record learning outcomes
As the weather gets colder, pharmacy customers may find that their skin feels drier, rougher and more irritated than usual. They may also seek advice on managing cracked lips and an itchy scalp. A change in skincare routine – and even switching to different products – may help to keep their skin hydrated at this time of the year.
“Dry skin can be quite a common symptom of winter weather,” says professor Carsten Flohr, consultant dermatologist and spokesperson for the British Association of Dermatologists (BAD).
“If you put together the drying effect of cold weather, indoor heating, and the fabrics that people use to stay warm and protect their skin, this can be a storm in a teacup for someone with a chronic skin condition. Eczema, for example, can become even drier and itchier in winter for some, so it’s important to know what your triggers are, and what you can do to relieve them.”
“Eczema can become even drier and itchier in winter for some”
Environmental changes
According to Dr Rakesh Anand, consultant dermatologist and British Skin Foundation (BSF) spokesperson, cold air holds less moisture than warm air, so when the temperature drops, the humidity in the environment falls too.
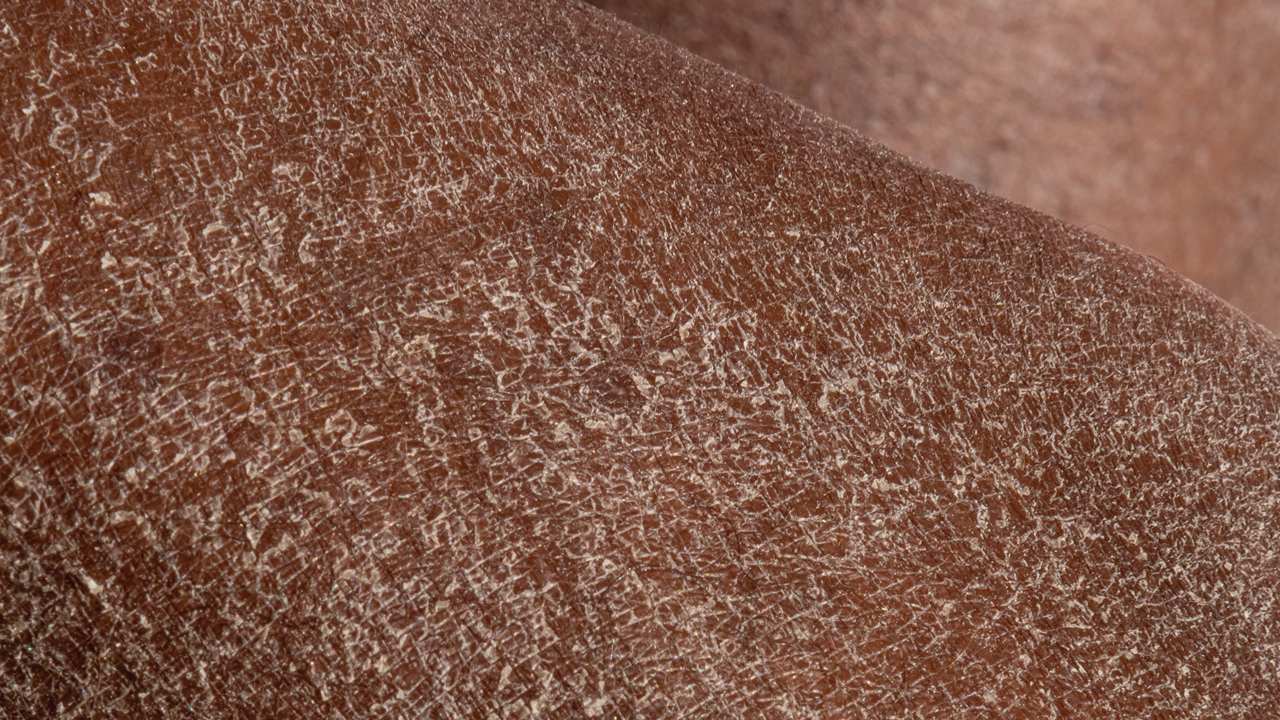
“This means water evaporates more easily from the skin’s surface, weakening the barrier and leading to dryness, flaking and irritation,” he says.
“At the same time, blood flow to the skin can decrease as the body conserves heat, which may make the skin appear dull or pale. Wind exposure further strips away surface lipids that normally help to keep the skin hydrated. Central heating, fan heaters and even long, hot showers all reduce indoor humidity, creating a very dry environment that accelerates water loss through the skin.”
Certain groups of people may be more prone to winter-related skin changes. Research published in the Dermatology and Therapy journal in October 2025 found that very low temperatures can cause symptom flare-ups in people with atopic eczema by increasing skin inflammation and affecting how well the skin barrier works.
“Those with eczema, psoriasis, rosacea or naturally dry and sensitive skin are particularly prone to barrier disruption and inflammation in colder months,” says Dr Anand.
“Most chronic inflammatory skin diseases either worsen or require more emollient care. Older adults are also more susceptible, as natural oil production and skin hydration decline with age.”
Julie Van Onselen, dermatology nurse adviser to National Eczema Society, says that indoor environments can dry out the skin as much as outdoor weather.
“A big factor is constantly moving between different temperatures, from the cold outdoors into central heating and back again,” she says.
“Using a humidifier at home may help to keep the skin hydrated. However, home environments aren’t the only problem. A child sitting by a radiator at school, for example, may have drier skin or even an eczema flare-up, if they’re prone to it. Older people in a care home can develop asteatotic eczema, which is worsened by over-washing and overheating in a warm environment.”

Applying an emollient before going to bed can help restore skin moisture.
Skincare regimes
During the winter months, pharmacy customers may need to make changes to their skincare regime to strengthen their skin barrier and help to combat the drying effects of harsher weather. With so many different skincare products available, customers will need to find the right combination to suit their needs.
“Switch to a gentle, fragrance-free cleanser rather than a foaming wash, and use a richer moisturiser that contains barrier-supporting ingredients such as ceramides, glycerin and shea butter,” says Dr Anand.
“Applying moisturiser immediately after bathing helps lock in hydration. Those using active ingredients such as retinoids may need to reduce frequency if sensitivity increases.
For very dry or cracked areas, overnight occlusion with a thicker ointment can help. It’s also worth reminding customers to avoid heavily fragranced or alcohol-based products, which can exacerbate irritation.”
Eczema patients may need to switch to a richer emollient, especially for parts of their body that are often exposed to the elements, such as their hands and face.
They should reapply the emollient more frequently than at other times of the year and make sure they are using a topical steroid as prescribed when a flare-up occurs.
“The best emollient is the one that suits that particular patient,” says Julie.
“Lotions are lighter and absorbed more quickly in the summer, but patients may need to step up to a cream or gel in the winter months. Most emollient brands include a range of different formulations, so it’s often straightforward to switch between the products at different times of the year.
Patients don’t necessarily need to step up to a greasy ointment, which most people don’t enjoy using. There’s also a fire risk with older people, in particular, if they are sitting by a fire with greasy emollient on their legs.”
Soaps and detergents can dry out the skin and cause irritation, so customers may need to switch to moisturising bath and shower products and reduce the water temperature.
“If someone is struggling with itchy and dry skin after washing, it may also be a good idea to change to a soap-substitute for these harsher months, especially for washing hands or in the shower,” says professor Flohr. “If dry skin is widespread and persistent, it’s worth seeing a GP about it.”
A moment on the lips
Lips are constantly exposed to the elements, making them prone to dryness, chapping, flaking and soreness during the winter months. Skin on the lips is much thinner than skin on the face and doesn’t have any oil glands, so it tends to dry out quickly and easily.
Licking the lips may seem to moisten them, but it actually dries out the skin even more. Covering the lips with a scarf when outside in cold or windy weather may help to reduce dryness, along with staying hydrated by drinking plenty of water.
Using a moisturising lip balm containing petroleum jelly, beeswax, cocoa butter or shea butter can help to combat dry lips – use this regularly during the day and in the evening before going to bed. Nice-smelling or coloured lip balms may seem like a treat, but some people are sensitive to certain ingredients.
Non-fragranced, plain emollient products are less likely to cause irritation or allergies. Most people need to use trial and error to see which product works well for them.
Dry lips can be a sign of an allergy or vitamin deficiency, or may be a side effect of some medicines (such as benzoyl peroxide used for acne), so it’s important to get it checked by a GP if the symptoms persist. Hot, painful, red and swollen lips may be a sign of an infection.
A small fluid-filled blister on a lip or around the mouth may be a cold sore. This is caused by the herpes simplex virus and may be triggered by stress or a respiratory infection.
A cold sore usually starts with a tingling, itching or burning sensation before the painful blister develops. The sore usually starts to heal within 10 days. It’s highly contagious during this time and can spread easily to other people, so good hygiene is important.
Customers can buy various cold sore products over the pharmacy counter, including creams to ease pain and inflammation, and cold sore patches to protect the skin while it heals. Antiviral cream needs to be used as soon as the tingling sensation begins – these creams don’t always work once the blister develops.
If a cold sore is very large or painful, or keeps coming back, customers should speak or their GP. They may need to take antiviral tablets.

“Dandruff, seborrhoeic dermatitis and psoriasis may also flare up at this time of year”
Self care advice
Most people opt for bulkier clothing during the winter, but wearing several thin layers that can be added or removed can stop overheating. When outdoors, pharmacy customers should cover parts of their body that are exposed to the elements, such as their hands. Gloves should be kept dry, however, as wearing wet fabric can lead to cracked skin.
Dry skin can also flare up on parts of the body that are usually covered by clothes. Some winter clothing can be particularly rough, especially if it’s made from wool (including socks and tights). Softer cotton or a natural, breathable fibre such as bamboo can be less irritating.
“The shins, in particular, are prone to dryness and irritation in winter,” says Dr Anand. “Thick clothing and heated environments can draw moisture from the skin. Wool or synthetic fabrics can also exacerbate itch and irritation, especially in those with eczema. Wearing cotton liners under woolen gloves can protect the hands.”
It’s tempting to keep doors and windows closed in colder months, especially if people don’t want to switch on the central heating, but inadequate ventilation means that house dust mites are more likely to thrive indoors.
This can trigger a flare-up of atopic eczema symptoms. If someone is prone to atopic eczema and spending more time indoors, the home may need to be vacuumed and damp-dusted at least once a day.
The National Eczema Society recommends keeping all of the rooms in the home at a regular temperature (ideally 18°C), placing a bowl of water near radiators to offset the drying nature of central heating, and not sitting too close to a heat source.
Some people find that their dry or inflamed skin flares up when they have a cold or flu, so keeping generally healthy is essential over the winter months.
To keep the skin hydrated, it’s important to drink plenty of fluids – ideally, six to eight glasses of water every day.
“Staying hydrated, eating a balanced diet with essential fatty acids, and continuing daily SPF use, even in winter, all help to maintain skin health,” says Dr Anand.
“Reassure customers that consistent care through winter will prevent the cumulative dryness that so often leads to flare-ups later in the season.”
Further support
Professor Flohr stresses that signposting pharmacy customers to accurate skincare information is essential. “Finding impartial advice in the internet age can be difficult,” he says.
“The British Association of Dermatologists publishes publicly available patient information leaflets (PILs) for a wide range of conditions, and can be found online. They even have QR codes for a patient to scan and read on their phones, if pharmacy teams want to share this in the pharmacy.”
The British College of Dermatology, the educational arm of the British Association of Dermatologists, has launched a series of online courses specifically written for community pharmacists, which has some information which may be relevant to the wider pharmacy team, too.
The courses tackle a number of relevant skincare topics including the management of eczema and psoriasis. They are available on the BCD Education Hub (bit.ly/4oWGMe2).
Pharmacy teams can also direct customers to relevant charities and organisations, such as the British Skincare Foundation (britishskinfoundation.org.uk), National Eczema Society (eczema.org) and Psoriasis Association (psoriasis-association.org.uk).
“Hot, painful, red and swollen lips may be a sign of an infection”
Scalp conditions
Cold weather can spell doom for scalp health, leading to dryness, itching and flaking. Wearing a hat or hood will protect the hair from wind, rain and snow, but a hot and sweaty head can exacerbate dryness and associated symptoms.
Using hairdryers or colouring, bleaching or perming products can also worsen scalp symptoms.It’s important to keep the scalp hydrated by using moisturising shampoos and conditioners.
Washing hair too often (more than two or three times a week) can strip the skin of its natural oils – and people should use gentle hair products (e.g. sulphate-free shampoo) if they need to wash their hair more frequently.
Long-term scalp conditions such as dandruff, seborrhoeic dermatitis and psoriasis may also flare up at this time of year, due to the cold, dry weather, tiredness and stress.
The symptoms of these conditions often overlap (redness, itching and flaking skin), but psoriasis tends to be more severe, causing sore, thick inflamed patches covered with silvery scales.
Some scalp treatments are available over the pharmacy counter for mild to moderate dandruff and seborrhoeic dermatitis. These include shampoos containing salicylic acid, zinc pyrithione, piroctone olamine, antifungal ingredients or coal tar.
Some of these products can be used regularly to prevent flare-ups. If the diagnosis isn’t clear, or the pharmacy products aren’t working, it’s important that customers are referred to their GP. Scalp psoriasis usually needs to be managed with prescribed treatments.