In Conditions
Follow this topic
Bookmark
Record learning outcomes
At a length of 6.7 metres and with a surface area the size of a tennis court, the small intestine – also known as the body’s ‘second brain’ – even has its own nervous system. So, it’s not surprising that it is susceptible to a whole host of health conditions.
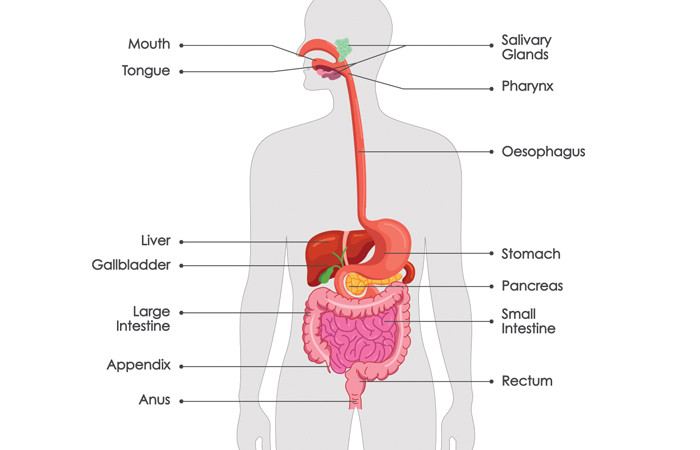
Gastrointestinal anatomy
To fully understand how the intestines work, it helps to have an awareness of the digestive system, from beginning to end. The ‘Love Your Gut’ initiative (loveyourgut.com/what-does-the-gut-do/the-digestive-system) offers this handy guide:
1. The mouth and teeth break food down into manageable pieces and mix these with saliva, which starts the digestive process
2. The oesophagus is the conduit between the mouth and the stomach. Swallowing initiates powerful muscular contractions that push food down into the stomach
3. The stomach secretes acid and peptic enzymes, which further dilute and break up food, killing off the majority of bacteria in food and delivering the resulting slurry into the small intestine in a regulated manner. It usually takes about one to five hours for most of a moderate sized mixed meal to be emptied from the stomach
4. The small intestine is a narrow tube about six metres long. Here, protein, fat and carbohydrate are broken down into amino acids, sugars and fatty acids, which are then absorbed into the bloodstream. It can take between two and four hours for a meal to be processed in the small intestine
5. The colon or large intestine salvages unabsorbed material from the small intestine. During a five to 70-hour residence, it extracts salt and water from the solidifying contents, while trillions of colonic bacteria ferment unabsorbed sugars, starches and proteins into short chain fatty acids (SCFAs), which are a source of energy
6. The pancreas is a digestive gland that secretes an alkaline juice containing powerful enzymes that break down protein, fat and carbohydrates. It is also the source of the hormone insulin
7. The liver receives blood from the gut, filters it, removes toxins, metabolises drugs, stores nutrients and synthesises proteins for various purposes including blood clotting. It also synthesises bile
8. The gall bladder stores and concentrates bile, and after a meal squeezes it into the small intestine, where it helps to digest fat.
“An unhealthy gut can lead to digestive disorders, fatigue and skin issues”
With all these component parts, it’s easy to see why pharmacy teams are called upon to help customers with advice and support for so many of the following common digestive problems.
Common digestive problems
Constipation
Constipation is a condition where the passage of waste through the bowels (the term used to describe the small and large intestine together) is slow, difficult to expel and sometimes painful.
Signs include abdominal discomfort, bloating, straining and a sensation that the bowels are never completely emptied.
The most common cause of constipation is excessive absorption of water by the colon. This can arise from insufficient fluid or fibre in the diet, a lack of exercise, certain medications, and illnesses that slow the passage of solid waste (stools) through the bowel.
Stress can also bring on constipation, as well as diarrhoea, and ignoring the urge to ‘go’ is another common a cause.
The first line of treatment for constipation is to increase fluid intake to at least seven to eight glasses daily, coupled with eating more dietary fibre and at least five portions of fruit and vegetables a day.
While regular use of laxatives is generally not recommended, occasional use is not harmful and a variety of over-the-counter (OTC) options are available.
Diarrhoea
Diarrhoea is common in adults and children. Often caused by a stomach bug, it usually stops within a week and is simple to treat at home.
The most important thing is to have lots of fluids to prevent dehydration, and to drink these in small sips to avoid feeling sick. There is no need to avoid any specific foods, but NHS advice is for sufferers to stay off school or work until they have not had diarrhoea for at least two days.
Taking paracetamol can help patients deal with discomfort, although product leaflets must be checked for age suitability and dosage instructions before giving paracetamol to a child.
If the person is showing signs of dehydration – such as dark, smelly urine – recommend oral rehydration sachets, or the customer can talk to the pharmacist about medicines such as loperamide to stop diarrhoea for a few hours (not suitable for children under 12).
Haemorrhoids
Haemorrhoids, commonly known as piles, are painful, itchy lumps that develop inside and around the anus. Symptoms include bright red blood after passing a stool, the feeling of not having completed a bowel movement, or slimy mucus in underwear or on toilet paper after wiping.
Piles often get better on their own after a few days, and there are several ways to prevent and treat them. Drinking lots of fluid and eating plenty of fibre will keep stools soft. Regular exercise and cutting down on alcohol and caffeine to avoid constipation can help too.
Sufferers can take paracetamol if the piles hurt. However, they should not take ibuprofen if their piles are bleeding or take painkillers that contain codeine, as these can cause constipation.
A variety of OTC products are available to treat piles locally. These contain ingredients like astringents, local anaesthetics and anti-inflammatories to reduce swelling.
Other digestive system disorders
- Irritable bowel syndrome (IBS) is a functional disorder with symptoms that include abdominal pain, bloating and changes in bowel habits, such as diarrhoea or constipation
- Crohn’s disease often presents with abdominal pain alongside diarrhoea, fever, weight loss and bloating
- Ulcerative colitis and other inflammatory bowel diseases can cause abdominal pain that varies with disease severity.
While many causes of abdominal pain are benign, some require urgent referral and treatment. For instance, severe or persistent pain can be a feature of more serious issues such as bowel obstruction or cancer and should be referred.
What's the difference? IBS vs IBD
Inflammatory bowel disease (IBD) and irritable bowel syndrome (IBS) are different conditions that need to be treated in specific ways.
Peter Whorwell, professor of medicine and gastroenterology at Manchester’s Wythenshawe Hospital, and author of Take Control of your IBS, explains:
“In IBD (Crohn’s disease and ulcerative colitis), the bowel is inflamed, whereas in IBS, the bowel is not inflamed and symptoms result from abnormal contractions of the bowel (‘disordered motility’) in conjunction with it being oversensitive (‘hypersensitivity’).
“Consequently, the treatment approach in IBD aims to reduce and control inflammation, whereas in IBS, treatment aims to control motility and reduce sensitivity.
Both conditions can cause abdominal pain, but most patients with IBD suffer from diarrhoea and seldom experience constipation, while in contrast, IBS can cause diarrhoea or constipation.”
Professor Whorwell says over-the-counter medications are “perfectly acceptable in IBS” and although they can sometimes make the patient’s symptoms worse, they “virtually never cause harm”.
However, pharmacy teams should be “extremely cautious” about recommending any medication for IBD, as there is “potential for causing serious harm”.
He continues: “For diarrhoea-type IBS, it is reasonable to offer an antidiarrhoeal such as loperamide or an enterosorbent such as Silicolgel or Enterosgel, both of which can ease pain as well as [improve] the diarrhoea and can be used long term.
Codeine has the advantage of reducing pain as well as diarrhoea, but causes dependency, so should not be used long term.
“In contrast, antidiarrhoeals should be used with extreme caution in IBD, as if the patient is in an acute attack, they can potentially cause life-threatening complications. They can sometimes be used in IBD patients in remission but should only be started by a specialist.”
Professor Whorwell describes antispasmodics as “extremely useful” for pain in IBS. “They target disordered motility and can be recommended by a pharmacist, GP or specialist,” he says.
“Laxatives are also extremely useful in constipation-type IBS and, contrary to popular belief, do not damage the bowel and can be use long term, and that includes the stimulant laxatives.”
He cautions, however, that NSAID medications can make both IBS and IBD worse, adding: “Paracetamol is the best analgesic in both IBS and IBD, and has no negative effects on the bowel.”

Bloating is a common symptom of abdominal discomfort and could indicate constipation, IBS, food intolerance or, in females, a more serious condition that needs investigation.
Bloating and gas
Dairy products can cause bloating, diarrhoea and gas – with many adults unaware they are intolerant to lactose, the natural sugar in dairy products.
Other foods that can cause issues are fried foods such as chips, burgers and sausages, which may either quickly move undigested through the body causing diarrhoea or stay in the digestive tract longer and cause bloating.
Julie Thompson, information manager at charity Guts UK, says: “Supporting customers to dietary adjustments such as regular eating patterns and ways to identify their triggers may also be helpful, and pharmacy staff can also recommend simethicone medicines for wind/trapped gas, and peppermint oil capsules or antispasmodics to ease cramping and discomfort.”
“Dairy products can cause bloating, diarrhoea and gas”
Digestive red flags
“Hydration, fibre and exercise are just a few of the measures which may help to relieve digestive symptoms,” says Julie. “But when red flags appear, it is always important to seek GP review, so remind customers that early investigation can often lead to better outcomes.”
For instance, while constipation is common and usually temporary, if it persists or is causing complications, it can lead to further problems.
“Signs that may require customers to contact their GP include simple treatments being ineffective and the bowel suddenly slowing up, especially in people over 40,” says Julie.
“Anyone experiencing unexplained weight loss, bleeding in the stool or rectal pain should be advised to contact their GP immediately.”
If customers have had diarrhoea for four weeks or longer, they need to see their GP so that the cause can be investigated. Vulnerable groups such as babies, young children and older people may also need medical advice sooner.
“If customers experience bloating, it is important they are aware of the red flag symptoms that suggest further investigations might be needed to rule out other conditions that can cause these symptoms.
These include unintentional weight loss; anaemia (a low blood count); a change in bowel habit (constipation and/or diarrhoea); loss of appetite; abdominal pain; or an increased need to pee,” says Julie.
“If customers were born female and have ovaries, they should also be tested for ovarian cancer if they have bloating. This can be arranged by their GP and is a simple blood test.”
With so many intestinal pitfalls and possible solutions, pharmacy teams are clearly a vital first line of advice and support when it comes to lower gastrointestinal health.
Getting to grips with gut bacteria
Stress, dietary changes, alcohol consumption, smoking, or medication such as antibiotics can create an imbalance in the microorganisms that live in our gut. These ‘gut microbiota’ support digestion and help to keep the gut healthy.
Thankfully, gut microbiota can be rebalanced through diet and supplementation with prebiotics, a type of dietary fibre that feeds the body’s natural microbiome, and probiotics, which add living bacteria to the gut.
But what’s the difference between prebiotics and probiotics?
“The gut microbiome is a collection of trillions of bacteria that have a huge impact on various parts of our health,” explains Mike Wakeman, clinical pharmacist and formulator of Evera Nutrition.
“Probiotics are live microorganisms that can benefit health when consumed in sufficient amounts; prebiotics are non-digestible fibres that feed and support the growth of these beneficial microbes (probiotics) in the gut.
“Then there are postbiotics, which are the by-products or inactive parts of these microbes. They can still have positive effects on the body, even though the microbes themselves are no longer alive.
“A diverse microbiome helps metabolise nutrients, produce certain vitamins and protect against harmful pathogens. An unhealthy gut, however, can lead to digestive disorders, fatigue and skin issues.
“The bidirectional communication pathway between the gut and the brain also means that the microbiome can affect neurotransmitter production. So, in essence, gut health underpins the body’s ability to extract and utilise nutrients, regulate immunity and inflammation and maintain mental balance.”
Further information
- Love Your Gut: loveyourgut.com
- Guts UK: gutscharity.org.uk/advice-and-information