Tumultuous times
In Conditions
Follow this topic
Bookmark
Record learning outcomes
It’s important for pharmacy teams to ensure that their knowledge of bowel conditions is up to date and to know when to refer customers to a GP for advice
It’s easy to take gut health for granted, until something goes wrong. Almost one in four people never think about looking after their digestive health, according to digestive disease charity Core. But a third of people regularly suffer from digestive complaints and 12 per cent of GP appointment time is taken up with digestive disorders, accounting for 14 per cent of the GP drug budget.

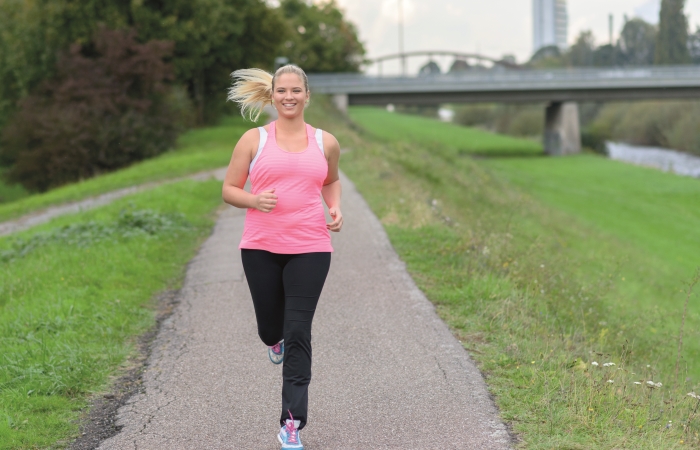
It would seem that few people have a good understanding of what constitutes a normal digestive system and how to keep the bowel healthy. For example, according to Bowel Cancer UK, 63 per cent of UK adults are not aware that being physically active for 30 minutes a day, five days a week, can cut the risk of bowel cancer. This highlights a need for awareness and education, which is where pharmacy can step in.
Irritable bowel syndrome Irritable bowel syndrome (IBS) affects around one in five people in the UK at some time in their lives, with more women affected than men, according to the IBS Network. It usually starts when the sufferer is in their teens or twenties and can come and go throughout life.
IBS is a chronic condition that causes problems with the function of the bowel, although the gut looks normal when examined. It can’t be cured, but there are lots of ways to manage and control symptoms.
The exact cause of IBS is not known, but it is thought to be linked with over-activity of parts of the bowel. Food passes along the bowel via contractions of the muscles of the bowel wall.
These contractions can become abnormal and this can cause pain and other IBS symptoms.
“People with IBS tend to have a sensitive gut, where symptoms may be triggered by diet, lifestyle or stress. By understanding these triggers and knowing what changes to make, people can often live well with the condition, given the right support and guidance,” says Ewa Gabzdyl, pharmacist and medical advisor to the IBS Network.
Intolerance to certain foods is thought to play a part in some cases. A bout of gastroenteritis may trigger IBS and it’s thought that bacteria in the gut could also be a factor.
The main symptoms
IBS symptoms vary from one individual to another. However, the main ones to recognise are:
- Stomach pain/cramps, which are often worse after eating and better after opening the bowels
- Bloating and swelling of the stomach
- Bouts of diarrhoea and constipation.
Other symptoms include: wind, nausea, tiredness, backache and needing to wee more frequently.
Treating IBS
“It’s really important to see your doctor to get a proper diagnosis,” says Ewa. “With wide variations in symptoms between individuals, and the fact that other conditions can masquerade as IBS, diagnosis is often challenging. Doctors will carry out a full medical history to identify any red fl ag indicators and help to screen other conditions.”
Managing IBS symptoms involves a mixture of medication and lifestyle and dietary changes. The main medication choices are:
- Antispasmodics, such as mebeverine or hyoscine, which relax the muscles in the gut wall and can relieve stomach pain
- Laxatives, such as docusate and senna, to treat constipation symptoms, if increasing fibre is not enough
- Antidiarrhoeals such as loperamide, when needed
- Peppermint oil to treat bloating and wind.
Lifestyle changes
“For people with IBS, it is worth considering physical activity levels and psychological wellbeing,” says Ewa. “Many people with IBS discover that their bowels seem to function like an emotional barometer. Emotional tension always makes IBS worse.” And, the way people eat is as important as what they eat. “Eat three regular meals a day, don’t skip meals or eat late at night,” advises Ewa.
There are also links between the brain and the gut. Stress and anxiety can cause IBS symptoms, so it’s important to make time to relax each day and to try therapies such as mindfulness and meditation. Customers should also ensure they get enough sleep, and seek support for managing stress and anxiety long term.
Diet tips
Before making dietary changes, advise customers to keep a food and symptom diary for a week to help identify any trigger foods: Ewa recommends making one change at a time so customers can see what works best for them. You can also advise sufferers to:
- Start with a balanced, healthy diet, with plenty of fruit and vegetables, dairy, protein and two litres of fluid a day
- Reduce caffeine as this can help with pain and diarrhoea symptoms. Coffee should be limited to a maximum of three cups a day
- Limit alcohol intake to no more than two units a day, with two alcohol-free days a week
- Cut down on fatty and processed foods
- Adjust fibre intake as required. Those with constipation may need to eat more fibre-rich foods and those with diarrhoea may need less
- Try probiotics as these may help to balance gut bacteria and improve diarrhoea, wind and bloating.
A special diet known as the low FODMAP diet has been shown to help around 70 per cent of IBS patients. FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides and polyols) are a group of short-chain carbohydrates that are poorly absorbed by the small intestine. They ferment easily and cause more fl uid to enter the large bowel, leading to gas, bloating and diarrhoea. These carbohydrates are found in a range of foods, including various fruit and vegetables, wheat and dairy products.
“It is recommended that anyone following this diet does so under the guidance of a specialist registered dietitian,” says Ewa.
Vitamin D and IBS
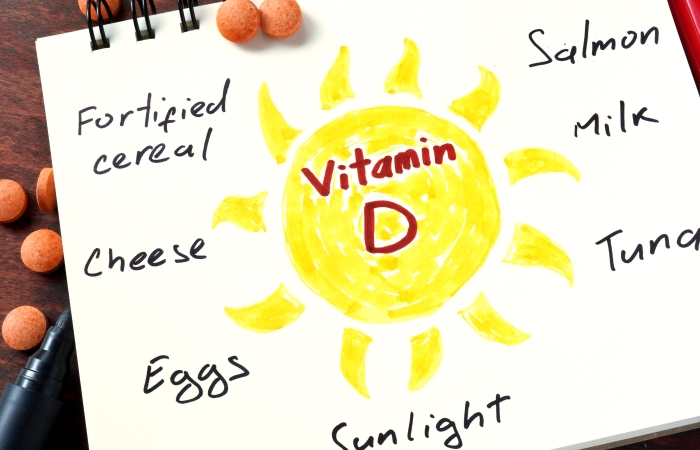
New research carried out at the University of Sheffield has found that IBS patients have a higher prevalence of vitamin D deficiency and that vitamin D supplements could potentially ease IBS symptoms.
“The study provides an insight into the condition and a new way to try to manage it. It is evident from the findings that all people with IBS should have their vitamin D levels tested and a large majority would benefi t from supplements,” said lead author Dr Bernard Corfe.
Ewa Gabzdyl, pharmacist and medical advisor to the IBS Network, agrees, adding: “Current evidence suggests that low vitamin D status is common among IBS patients. This merits assessment of vitamin D levels and, if needed, rectifi cation for general health reasons.”
Inflammatory bowel disease
Inflammatory bowel disease (IBD), which includes ulcerative colitis and Crohn’s disease, affects at least one in 250 people in the UK and is increasing in prevalence. Most patients are diagnosed in their teens and twenties and at least 300,000 people are affected in the UK, according to the charity Crohn’s & Colitis UK. Patients with IBD also have an increased risk of bowel cancer.
- Crohn’s disease
This condition causes inflammation of the digestive system and can affect any part of the gut. The common signs are diarrhoea and abdominal pain, tiredness, mouth ulcers, loss of appetite, weight loss and anaemia. It affects 115,000 people in the UK. Often inherited, Crohn’s can be triggered by a virus, diet, smoking or stress. Treatment is with medication, surgery or both. - Colitis
This causes inflammation and ulceration of the lining of the large bowel. Symptoms are diarrhoea, cramping pains, tiredness, loss of appetite, weight loss and anaemia. It affects one in 420 in the UK and is usually diagnosed between the ages of 15 and 25.
Colitis is thought to be caused by genetics, combined with an abnormal reaction of the digestive system to bacteria in the gut and a trigger, such as a virus or infection. It is usually managed with medication.
People with colitis should be screened for bowel cancer from 10 years after diagnosis and every three to five years thereafter.
Bowel cancer
Bowel cancer is the fourth most common cancer in the UK, with 41,200 people diagnosed each year, according to Bowel Cancer UK. Over 90 per cent are aged over 50, but it can affect people of all ages. Around 16,000 die from the condition every year, making it the second most common cause of cancer death after lung cancer. Symptoms include:
- Bleeding from the anus or blood in the stools
- A persistent change in bowel habit
- Unexplained weight loss
- Extreme tiredness
- Pain or a lump in the tummy.
To reduce their risk of bowel cancer, customers can be advised to:
- Take regular exercise: 150 minutes of moderate activity each week can cut the risk of bowel cancer by 12 per cent
- Reduce drinking: some 11 per cent of bowel cancers are linked to alcohol
- Give up smoking: eight per cent of bowel cancers are linked to smoking
- Improve diet: limit red meat intake to 500g a week and avoid processed meats altogether. Eat at least 30g of fibre a day and drink plenty of fluids to keep the gut moving
- Maintain a healthy weight: some 13 per cent of bowel cancer cases are linked to being overweight.
Common conditions
Diarrhoea
The most common cause of diarrhoea is an infection of the gut – usually gastroenteritis. This can result from eating infected food or, in some countries, drinking infected water. Other less common causes are IBS, medication or ulcerative colitis. The main symptoms are loose stools, cramping pains, a fever and headache.
Most cases of diarrhoea can be safely treated with OTC products. Customers who may need to be referred to the pharmacist include those who have been abroad recently; those who’ve been in contact with anyone with similar symptoms, and those who have been on antibiotics or recently had a hospital stay. Customers should also be referred if they are severely dehydrated; unable to keep fluids down; have blood in their diarrhoea or vomit, a persistent fever or a weakened immune system.
Treatment
It’s essential to prevent dehydration by drinking more fluids than usual. An extra 200ml after each bout of diarrhoea is recommended. Oral rehydration sachets help to replace lost fluids and salts.
The guidance is to eat small, light meals and not avoid eating, if possible. Plain foods such as rice or wholemeal bread are easy to digest.
Antidiarrhoeals such as loperamide can be used to shorten an attack if necessary.
To stop the spread of diarrhoea, advise customers to:
- Wash their hands thoroughly after using the toilet and before eating or handling food
- Not share towels and/or flannels
- Not prepare or serve food for others
- Regularly clean toilets
- Stay off work/school until 48 hours after the last episode.
Constipation
There can be many causes of this common bowel complaint and these include lack of fi bre, not drinking enough water, some medications (e.g. iron tablets, codeine and some antidepressants and antacids), an underactive thyroid, IBS and pregnancy.
Treatment
Increasing fibre intake adds bulk to stools. Customers should aim for at least five portions of fresh fruit and vegetables a day. Whole grain breakfast cereals, brown rice and wholemeal pasta are other good sources. In addition, advise customers to:
- Aim for at least two litres of fluid a day
- Take regular exercise to keep the gut moving
- Don’t ignore the urge to empty bowels.
If lifestyle and diet changes don’t help, occasional use of laxatives can be recommended. A bulk-forming laxative (e.g. ispaghula, methyl cellulose, sterculia) helps stools retain fluid. A stimulant laxative (e.g. senna, bisacodyl, docusate sodium) stimulates the nerves in the large bowel. An osmotic laxative (e.g. lactulose, macrogols) works by retaining more fluid in the bowel.
Wind and bloating
Wind is caused by a mixture of gasses – from the air swallowed when eating and from stomach acid produced during digestion. Bloating can be a sign of IBS, indigestion or constipation. It can also be caused by lactose intolerance, fructose intolerance and some medications (e.g. metformin, lactulose).
Treatment
Customers should be advised to keep a food and symptom diary to fi nd out if they may be intolerant to any foods, as well as avoiding gas-producing foods such as sprouts, cabbage, onions, leeks, garlic, beans and lentils and foods containing sorbitol. They should also reduce consumption of fizzy drinks.
Regular exercise can help to relieve bloating and wind. If this doesn’t work, simeticone can help to break up gas bubbles and charcoal remedies work by absorbing gas. Antispasmodic treatments (e.g. mebeverine, alverine) can also help to relieve bloating.
Bowel cancer is the fourth most common cancer in the UK, with 41,200 people diagnosed each year
