In In-depth
Follow this topic
Bookmark
Record learning outcomes
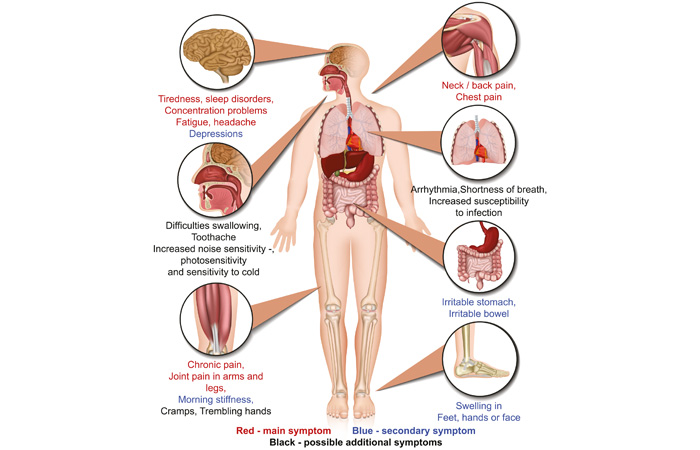
Fibromyalgia is a chronic condition of widespread body pain and fatigue, associated with multiple other physical symptoms as well as cognitive symptoms such as poor memory and concentration. Yet, despite figures from charity Versus Arthritis showing that between 1.7 to 2.8 million adults in the UK have fibromyalgia – around one in every 20 people – the condition seems to incite the same level of scepticism and disbelief as chronic fatigue did a few decades ago. So, what is fibromyalgia, and how can pharmacy teams support customers who are living with it?
Common risk factors
Fibromyalgia prevalence increases with age, and it is more common in women than in men. According to Versus Arthritis, fibromyalgia develops because of a combination of biological, psychological and social factors, and often accompanies some other common comorbidities. For example, depression and anxiety are more prevalent in people with fibromyalgia than in those without, fibromyalgia is associated with a 1.54-fold increased risk for irritable bowel syndrome, and it is more common in people with chronic back pain and rheumatic diseases such as rheumatoid arthritis, psoriatic arthritis and spondyloarthritis.
Getting a diagnosis
Gabriella Pearson is the co-founder of The Menstrual Health Project, a UK charity focused on improving education on both menstrual health and women’s health concerns and conditions. She was diagnosed with endometriosis at 23, adenomyosis at 24, and fibromyalgia at 30, and says getting an initial diagnosis is not easy.
“My GP is very proactive and diagnosed me with fibromyalgia by a process of elimination with blood tests, symptoms and looking at other factors, but I know that’s not everyone’s fibromyalgia journey,” says Gabriella. “I think success in getting a diagnosis varies between health boards and a lot of people will be and have been turned away, essentially being told the pain is in their head, that it could be other things or just to get on with it. I also think there is a big culture of misdiagnosis when it’s anything to do with pain, fatigue and mental health, but I would say if anyone’s looking to get diagnosed, find out if you have a pain management team within your health board that you can be referred to, to see kind of what options are available.”
Living with fibromyalgia
Fibromyalgia in itself is not thought to cause any lasting damage to body tissues. However, because there is no specific treatment for the condition, and pain and fatigue lead to low physical activity levels which then cause muscle weakening, sufferers can end up in a vicious cycle of worsening pain, fatigue and poor mental health.
After being diagnosed with fibromyalgia in February 2023, Gabriella says: “Living with fibromyalgia is really difficult, both physically and mentally, especially when trying to manage it alongside my other chronic health conditions. I have struggled with widespread pain, chronic back pain and migraines, and mental health issues, and the fibromyalgia symptoms have severely impacted my daily life, leading me to leave my job due to the pain and fatigue. I’ve also found it challenging to get proper support and management for my fibromyalgia, including being discharged from pain management without my knowledge, and not having a clear treatment plan.”
Lifestyle advice
When it comes to lifestyle advice that pharmacy teams can give to patients living with fibromyalgia, Mark Burdon, pharmacist at Burdon Pharmacy Group in Newcastle-upon-Tyne and advisor to Deep Heat and Deep Freeze, says a multi-faceted approach can help them manage symptoms and improve their overall quality of life.
“Encouraging a healthy lifestyle is a good place to start,” says Mark. “Recommend a balanced, nutritious diet to help manage inflammation, and advise on the importance of regular, gentle exercise like walking, swimming, or yoga to improve fitness and pain management.”
“Pharmacy teams can also suggest trying to maintain good sleep habits, as fatigue is a common symptom of fibromyalgia, and highlight the potential benefits of vitamin D – and getting vitamin D levels tested – since vitamin D deficiency can present with similar symptoms to fibromyalgia.”
Pain management strategies will vary from person to person, but Mark stresses that pharmacy teams should “advise against over-reliance on painkillers, as this can lead to dependence”. Instead, he says: “Suggest exploring alternative pain relief methods like topical creams, heat and/or cold therapy, or transcutaneous electrical nerve stimulation (TENS), and recommend cognitive behavioural therapy (CBT) to help manage pain and fatigue.”
Medical cannabis treatment
Several studies have produced promising findings on the effect of medical cannabis on fibromyalgia. However, there remains a lack of high-quality research, such as randomised controlled trials, which are necessary to determine its effectiveness and safety.
In 2019, Curaleaf Clinic (formerly Sapphire Medical Clinics) launched the UK Medical Cannabis Registry to collect data on the outcomes of patients prescribed cannabis-based medicines for a variety of conditions, including fibromyalgia. A recent study analysed data from the Registry, focusing on fibromyalgia patients who were prescribed medical cannabis for at least 12 months, and found that patients reported significant changes in pain, sleep quality, and overall wellbeing after starting medical cannabis. The study also showed a significant change in prescription opioid use among patients prescribed medical cannabis.
While more research is needed to determine its efficacy and safety, Curaleaf Clinic says these findings are “particularly significant” for patients who haven’t found relief from traditional treatments for fibromyalgia symptoms, as they may be potential candidates for medical cannabis therapy after evaluation by a specialist.
Lived experience
Nonetheless, for many people, finding what works best to manage their symptoms is a process of trial and error.
“I think it’s really hard to kind of give generic advice, because I don't think conditions like fibromyalgia are one size fits all,” says Gabriella. “I've personally found that things like TENS machines and gadgets like that don't work for me because I feel like it inflames my pain more, although I bought some electric heat pads online for about £15-£20 and they are absolutely fantastic and one of the best investments I’ve made.
“I also use compression socks and gloves, and I find sitting with my legs elevated helps a lot. I keep a portable bed pan in the car, because you can suffer with bowel issues when you have fibromyalgia, and I use a walking stick as and when I need it, and a wheelchair as well. I think younger people especially don't think they're ‘allowed’ to use mobility aids, but I've really found these things helpful to try and conserve my energy and not get to a state of fatigue. Minimising stress and maximising sleep is another thing to consider – if I’ve got an event coming up, I try and get more sleep to avoid fatigue and feel as refreshed as possible. It’s about looking at what areas you're struggling with and working out how to lessen their impact.”
Pharmacy advice and support
As the front door to the NHS, if community pharmacy staff can encourage and support patients to access and work closely with the wider primary care team, this can make a big difference to people who are living with chronic pain and fibromyalgia.
“Pharmacy teams have a vital role to play in helping patients access appropriate healthcare resources so they can understand what is available to them,” says Mark. “For example, healthcare professionals such as rheumatologists or specialists – and, of course, GPs – can provide more comprehensive care and support for managing chronic pain conditions like fibromyalgia.”
Emotional support and validation can also make a huge difference to patients, especially for people living with ‘hidden’ conditions such as pain.
“People living with chronic pain often feel they are being fobbed off or not taken seriously, which can be very frustrating,” says Mark. “It’s really important that pharmacy teams can listen to the patient's experiences without judgement, taking time to really hear and understand their perspective, and validate their concerns.”
Gabriella agrees: “There’s still a big stigma around fibromyalgia, and of all the conditions I’m living with, it's been the hardest one to come to terms with. Unfortunately, because there aren't surgeries or procedures that can relieve fibromyalgia like there are for conditions such as endometriosis, I still feel that the pathway and the guidelines and the support for fibromyalgia isn’t where it should be and when you get diagnosed, you’re very much left to your own devices to deal with it.
“People also forget how many different layers there are to conditions like fibromyalgia,” she adds. “I think one of the most important things people can do – whether it’s friends, family, medical professionals, pharmacy support staff, whoever – is just to listen and not have judgment, because everyone's journey and what they are experiencing with fibromyalgia is really different. And if you don't know about a condition or what someone says they are experiencing, don’t be afraid to read up about it or ask them questions, rather than simply making assumptions. Just because you can’t see a person’s pain doesn’t mean they’re not going through it.”
Further information
- HCPS can request a Fibromyalgia Action UK Health Professionals Pack at: fmauk.org/useful-information/658-have-a-medical-pack-sent-to-your-gp-or-medical-professional
- Menstrual Health Project: menstrualhealthproject.org.uk.

