In In-depth
Follow this topic
Bookmark
Record learning outcomes
In a world where information is freely available at our fingertips, wellness influencers are a dime a dozen and a new health documentary comes out every year, you’d think we would have a pretty good hold on our health. Yet, whilst there is an abundance of information available, there is little evidence to suggest that the correct information is being consumed, and when it is, being understood.
State of the nation
The ‘British Dietary Habits and Declining Nutrient Intakes’ review published by the Nutrition and Food Technology journal in September 2024 and the Health and Food Supplement Service (HSIS) Decades of Decline 2024 report both found that not only are people unsure of what makes up a healthy diet, but that this is worryingly reflected in the falling nutrient levels of the UK public – the impacts of which are linked to increased prevalence of multiple chronic illnesses, widespread weakened immunity and immense added strain on the NHS. “Unhealthy diets, which are common in the UK, account for 13 per cent of all deaths,” the Decades of Decline 2024 report states. “Most of this is because poor diets cause obesity, high blood pressure, high blood cholesterol and type 2 diabetes. Obesity is also linked to 13 different cancers.”
The ‘British Dietary Habits’ review looked at data from the National Diet and Nutrition Survey (NDNS), that assesses diet, nutrition intakes and nutritional status of the general UK population each year. “The NDNS shows that intakes of a number of important micronutrients are falling, in some cases at an alarming rate,” says Dr Nisa Aslam, a GP from the HSIS and co-author of the review. “And despite the huge sums of money the Government, NHS and other organisations have spent on awareness campaigns, almost two in five adults don’t know about the Eatwell Guide on the proportions of each food group recommended for a healthy diet.”
The ‘British Dietary Habits’ review also assessed findings of the HSIS Survey 2024, which asked participants about dietary habits, attitudes, vitamin and mineral intake, and the perceived nutritional level of their diet and if they thought there was room to improve. Carrie Ruxton, a dietician from the HSIS, expressed concerns over the education gaps the survey highlighted, saying: “The data suggests that too many Brits are blind to the importance of a nutritious diet, and are confused about how to eat healthily” – confusion which is likely to reveal itself down the line in risks of serious health issues like heart disease, diabetes and stroke. Furthermore, the Decades of Decline 2024 report assessed the new research and found that of adults in the UK, worryingly:
- 43 per cent are experiencing tiredness
- 39 per cent report anxiety
- 33 per cent suffer low energy levels
- 28 per cent complained of low mood
- 27 per cent reported sleeping issues.
“Unhealthy diets, which are common in the UK, account for 13 per cent of all deaths”
What’s the damage?
The research from the Decades of Decline 2024 report revealed falling nutrient levels of many vitamins and minerals. Since 2008, vitamin A intakes have declined 21 per cent in children, 23 per cent in teens, 13 per cent in working-age adults, and 29 per cent in over-85s. Resultingly, 10 per cent of adults aged 19-64 and one in five of 11 to 18-year-olds have vitamin A levels below the Lower Reference Nutrient Intake (LRNI) – the amount of a nutrient that is sufficient for only 2.5 per cent of the population.
Vitamin D intakes have also declined since 2008. One in five people in the UK are deficient, “with much more serious shortfalls in some demographics” says the report. Two in five girls (39 per cent) and 15 per cent of boys aged 11-18 are deficient, with 19 per cent of working-age women and 16 per cent of working-age men also being deficient.
Calcium levels have fallen by 20 per cent over the last 20 years, the report states, with almost one in seven working-age adults and 15 per cent of 11 to 18-year-olds with calcium intakes below the LRNI.
“Among young girls and women, this rises to one in five and in women aged 19-64, the numbers of women failing to achieve this dietary target has climbed steadily from six per cent to 11 per cent,” says the report. Women with “dangerously low folate [folic acid]” is now at 90 per cent.
Iron, iodine, magnesium, potassium, omega-3 fatty acids and selenium have all seen worrying declines either overall or in specific age groups.
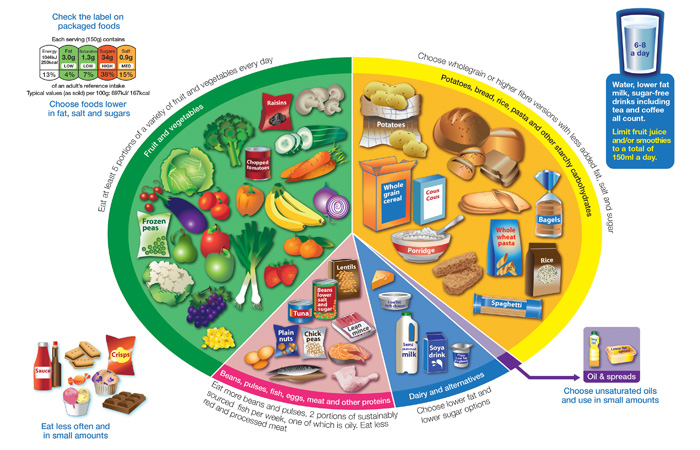
The Eatwell Guide is the NHS’s official recommendation of how much of what we eat overall should come from each food group for a well-balanced diet.
What’s to blame?
Various factors contribute to these falling nutrient levels. The Decades of Decline 2024 report includes research into consumer attitudes towards diet and nutrition. It found several potential drivers for deficiencies. One of the most notable are diets that exclude whole food groups. The report found that, of respondents:
- 78 per cent were meat eaters
- Nine per cent were vegetarian
- Six per cent were pescatarian
- Three per cent were vegan, with this more common in women than men (three per cent and two per cent respectively)
- The remainder were lacto-ovo vegetarians or did not follow a specific eating pattern.
“Meat is a source of highly bioavailable iron and zinc, so avoiding meat is undoubtedly a factor in the poor iron and zinc nutrition in these survey participants,” says Dr Aslam. “Iron from plant foods such as beans, lentils and vegetables are not so well absorbed as that from meat, and although vitamin C helps the absorption of iron from plant foods, this research indicated that the required knowledge and food preparation skills were lacking.” This highlighted another reason for declining nutrition. “A lack of knowledge is a key reason for the nutrient decline observed in the HSIS report. A total of 85 per cent don’t know the recommended intake for nutrients, and a large proportion have little idea of how nutrients function in the body”, Dr Aslam continues, so lack of education is also a huge driver for deficiencies.
“Other factors contributing to nutrient decline include fad diets, efforts to lose weight –which might be necessary but [reduces] energy and nutrient intakes – lack of time, skipping meals and being sufficiently organised to prepare healthy food and meals. Increasing cost of healthy food is also a factor.” Dr Aslam also notes that 41 per cent of consumers say cost is the most important factor when purchasing food. Nutritional factor was the decider for just 21 per cent of consumers.
“The World Health Organization has identified unhealthy diets as one of the most serious global risks to health”
Implications
Falling nutrient levels have an array of implications. The World Health Organization has identified unhealthy diets as one of the most serious global risks to health and emphasises the need for a nutritious diet to reduce risks of heart disease, stroke, diabetes and cancer. Heart and circulatory diseases which kill 480 people annually, “account for 270 hospital admissions and impact the lives of 7.6 million people. The British Heart Foundation estimates the immediate healthcare costs are around £10 billion each year”, the Decades of Decline 2024 report states.
Poor diet – and obesity – is also linked to type 2 diabetes. Poor dietary habits, like skipping breakfast and snacking, have been associated with a heightened risk of diabetes, another major public health challenge which heavily impacts healthcare services.
Osteoporosis impacts one in two women and one in five men over 50 in the UK, which has some of the highest rates of the condition in Europe. Public health nutritionist and part of the HSIS expert panel, Emma Derbyshire, put this into perspective: “Women over the age of 45 will spend more days in hospital due to osteoporosis than they will for diabetes, heart attack or breast cancer, and every month 1,150 people die following a hip fracture.” The associated healthcare costs for hip fractures are £5 million a day, and £2 billion a year. Although osteoporosis predominantly affects people aged 50 and over, it is during childhood, adolescence and early twenties where one builds up optimal bone density. “We also know that a diet that is deficient in bone-building nutrients, particularly between the ages of 10-20 years, can result in lower peak bone mass,” says Carrie. This makes it exceptionally important to address calcium and other deficiencies in younger people to avoid large numbers of people suffering from osteoporosis in the next few decades and circumvent preventable pressure on the NHS.
Lastly, the nutrient intakes in women are particularly a cause for concern, with “almost 90 per cent of women [having] dangerously low folate intakes sufficient to risk giving birth to a baby with a neural tube defect,” says Dr Aslam. “Women with low intakes [of iodine] during pregnancy risk the health of their unborn baby.”
Sifting through misinformation
Evidently, the population are struggling to digest information around healthy eating. “The HSIS report pointed to the need for clear information on nutrition as four out of five (83 per cent) are confused as to what a healthy diet looks like,” says Dr Nisa Aslam, a GP from the Health and Food Supplement Service (HSIS). This may be due to a host of reasons, one of them being the abundance of information available online. It can be difficult for non-healthcare professionals to separate the facts from the fiction, as oftentimes information appears to be well-informed, containing a kernel of truth which makes readers or listeners believe in it. And while it can be easy to accept information that aligns or reaffirms one’s beliefs, pharmacy teams should encourage customers to consume healthcare advice objectively and put further research into trusted sources, such as the NHS website. When absorbing information, encourage customers to:
- Consider where the information is coming from. What are the author’s credentials (have they published other healthcare articles?), what is their motivation for writing/sharing this information, if it is a website, is it a trusted domain e.g. ‘.edu’ or ‘.gov’?
- Read beyond the headlines. Does the supporting information reinforce the statement?
- Check the date – some people may share content that is years old and is now outdated
- Use an objective lens. Consider if your own beliefs may be affecting your enthusiasm or hesitancy to believe a claim
- Ask a healthcare professional if you are unsure if something is true. If you have applied the first few points and still cannot tell if something is true and are considering implementing it in your lifestyle, check with an expert first.
In general, when it comes to diet, Dr Aslam reaffirms that “healthy eating involves basing meals on sources of protein such as beans, lean meat or fish (including oily fish) with whole, high fibre grains, fruit and vegetables (five-a-day) and some dairy or plant-based equivalent with a few nuts and seeds. Such a diet should provide nutrients in sufficient amounts but it does take time to adopt such a diet. A multivitamin and multimineral supplement helps to bridge this nutrient gap.” Pharmacy teams are vital resources in signposting customers to trusted sources surrounding their diet and nutrition, which include to a dietician or GP.
How can pharmacy help?
It is crucial that people are encouraged to make more conscious efforts to improve their nutrient intakes. However, the other side of the coin points to re-thinking messaging from Government and/or healthcare bodies around nutrition. Currently, the message being put forward is that the public can obtain most of their nutritional needs from their diet and through the five-a-day recommendation (eating five portions of fruit and/or vegetables a day). Real-world research conducted by the HSIS has shown that unfortunately, even when people are aware of this recommendation, they are unable to put it into practice due to time constraints, cost of food or lifestyle choices. “Knowledge needs to increase, and the person needs to understand the relevance of knowledge to their own diet and lifestyle,” says Dr Aslam. “A multivitamin and multimineral is effective for bridging this dietary gap while the diet is being improved. If you avoid any food groups, are cutting calories to try to lose weight, skip meals or don’t eat five portions of fruit or vegetables every day, there is a strong argument for taking a multivitamin and multimineral supplement to help prevent any potential dietary deficiencies or shortfalls.” It is recommended that people living in the UK take a daily vitamin D supplement of 10mcg during the winter months when sunlight is limited.
Dr Aslam recommends suggesting the Eatwell Guide to customers to gain an understanding of what a well-balanced diet consists of. With this in mind, consumers can make educated choices when it comes to picking their produce. While not the only factor leading to increased risks of conditions like osteoporosis or diabetes, diet remains “a cornerstone for maintaining optimal health”.

